1. Executive Summary
1.1 Introduction
Calderdale and Huddersfield NHS Foundation Trust (CHFT) is an integrated Trust that provides acute and community health services. Hospital services are provided at Calderdale Royal Hospital (CRH) and at Huddersfield Royal Infirmary (HRI). The distance between the two hospitals is just over five miles. The Trust provides community services in the Calderdale area.
Clinical, workforce and financial risks have been identified if there is no change to the current configuration of services. These risks and their potential solutions have been debated for a number of years. This includes formal public consultation on proposed future arrangements for the configuration of services during 2016, referral of the proposals to the Secretary of State for Health and Social Care by Calderdale and Kirklees Joint Health Scrutiny Committee in 2017 and review of the proposals by the Independent Reconfiguration Panel in 2018. Whilst the Trust has day to day operational plans in place to ensure the care and safety of patients, a sustainable solution is urgently needed.
This Strategic Outline Case (SOC) addresses feedback from staff, patients and the public and the recommendations of the Independent Reconfiguration Panel (IRP). The Trust has the opportunity to reshape services, a track record that demonstrates capability to deliver, and a clear proposal which provides the basis for delivering safe, sustainable services.
The West Yorkshire and Harrogate Health and Care Partnership has confirmed that the proposals described in this SOC fit with the overall strategy for the development of better health and care services for West Yorkshire and Harrogate and that these proposals are their highest priority for public capital investment. In December 2018 the Department of Health and Social Care (DHSC) announced that 100% public capital funding of £196.5m had been allocated to support implementation of the proposals described in this SOC.
1.2 Strategic Context
People in Calderdale and Huddersfield are living longer. More people are likely to have multiple long term conditions thereby increasing the demand on the health and social system.
Nationally growing shortages of qualified clinical staff has increased use of agency and other temporary workers to fill vacancies, and this has increased NHS expenditure and made services less stable. This national workforce pressure is exacerbated at CHFT with the current two site configuration of most services, making it difficult to recruit and retain staff leading to a reliance on temporary and agency staffing to sustain service delivery.
CHFT has consistently delivered a high level of performance against national access targets and was given an overall rating of "Good" by the Care Quality Commission (CQC) in 2018 (this combined rating included "Requires Improvement" for the Use of Resources). Over the last two years across the combined and ranked metrics of Referral to Treatment Times (RTT), Emergency Care Standard (ECS) and Cancer waiting time less than 62 Days, CHFT has consistently been one of the best performing Trusts in England.
CHFT is one of the most digitally advanced Trusts in the country and this is key to enabling delivery of high standards of performance. However ensuring delivery of high standards of performance is fragile as the current dual site configuration is reliant on continued use of agency and temporary staffing (and the higher costs associated with this).
The Trust carries a very high risk in terms of the condition and reliability of buildings at Huddersfield Royal Infirmary (HRI). Overall the estate is in poor condition with significant backlog of maintenance for time expired buildings. There are statutory requirements across the site that demand immediate remedial action and a significant investment is required to resolve the functional suitability of the estate, with some buildings not clinically fit for purpose.
The Trust has a financial deficit and is reliant on financial support from the Department of Health and Social Care (DHSC). Structural costs associated with the dual site configuration of services (which require higher workforce expenditure) is a key factor driving the underlying deficit.
1.3 Clinical Case for Change
There is a compelling clinical case for the reconfiguration of the Trust’s services to improve the safety and quality of services and ensure the sustainable provision of acute and emergency services in the future. The current dual site model of hospital services does not, and cannot, meet national guidance.
A number of independent reviews and inspections of services have recommended that the status quo (i.e. to do nothing) is not an option and that changes to the configuration of services are needed to improve outcomes and safety. This includes: the National Clinical Advisory Team; the Calderdale Council People’s Commission; the Royal College of Physicians; Yorkshire and the Humber Clinical Senate; NHS England (NHSE); NHS Improvement (NHSI); the Independent Reconfiguration Panel (IRP), the West Yorkshire and Harrogate Health and Care Partnership, and; the Calderdale and Kirklees Joint Health Scrutiny Committee.
1.4 Future Hospital Services Model
The proposed future model of hospital services will support and enable delivery of the vision and ambitions described in the NHS Long Term Plan that was published in January 2019. Digital technology will have a central role in transforming services supporting more people to have care at, or closer to, home. This will be complemented by a hospital model that provides essential clinical adjacencies and the critical mass required to sustain staff recruitment and retention, ensure quality and deliver revenue savings.
The proposed model will make use of both existing hospitals. Both sites will provide 24/7 A&E services and a range of day-case, outpatient and diagnostic services - although whenever possible, services will be delivered in the community and closer to people’s homes. The total number of hospital beds will remain broadly as they are now whilst services are developed in the community and demonstrate a sustainable reduction in the demand for in-patient hospital care.
- HRI and CRH will provide 24/7 consultant-led A&E services;
- A&E at CRH will receive all blue light emergency ambulances for patients that have serious life-threatening conditions and all patients likely to require hospital admission;
- CRH and HRI will provide medically led 24/7 urgent care;
- Critical care services, emergency surgery and paediatric surgery will be provided at CRH;
- Physician-led inpatient care for people who do not require the most acute clinical inpatient healthcare will be provided at HRI;
- Midwifery led maternity services will be provided on both hospital sites;
- Consultant-led obstetrics and neo-natal care will be provided at CRH;
- Planned surgery and care will be provided at HRI.
- Patients that require complex surgery or it is known that they will require critical care after surgery will be treated at CRH.
- Digital Health capability, such as the electronic patient record and patient portals will enable ‘real-time’ review and advice on patient’s care to be provided by specialist staff where required.
1.5 Estate Plan
The West Yorkshire & Harrogate Health and Care Partnership has agreed the proposals described in this SOC as their top priority for capital funding and the DHSC announced in December 2018 that 100% public capital funding of £196.5m has been allocated to support implementation of the proposals. This will be used for:
- £20m investment at HRI to enable adaptation of existing buildings and to address the most critical backlog maintenance requirements enabling the continued use of some buildings on the HRI existing site.
- £177m for expansion and new build at CRH.
These proposals do not fully address the backlog maintenance requirements at HRI and the Trust will therefore continue to manage a very high risk in terms of the condition and reliability of buildings at HRI.
1.6 Economic Case
An assessment of the financial and non-financial benefits of the proposed service and estate model compared to continuing the existing service model and, in relation to the capital funding source, has been undertaken. The Economic Case analysis demonstrates the case for change and that the proposed service model provides economic, value for money (VFM) advantage compared to the existing service model.
1.7 Financial Case and Affordability
The financial case demonstrates affordability of the investment into the Trust’s estate and reconfiguration of services. The modelled clinical activity and revenue has been agreed as affordable for the local health sector and this is confirmed by Greater Huddersfield and Calderdale Clinical Commissioning Groups (CCGs).
The investment provides medium term sustainability for the Trust and mitigates significant estate and service risk that exists within the Business As Usual and the Do Minimum case. The Agreed option delivers a net £10m financial efficiency and sees the Trust return to financial balance without Financial Recovery Fund revenue in FY27. The cumulative deficit position is favourable at FY27 compared with both the Business As Usual and the Do Minimum options and this position improves further at FY45.
1.8 Stakeholder Engagement
This SOC builds on significant public, stakeholder and clinical engagement since 2012. This SOC is an evolution of the proposals informed by the extensive previous clinical and public engagement and the formal public consultation undertaken in 2016. There are a number of areas where the proposed service model is unchanged from that which was previously the subject of public consultation. Where changes have been made these have sought to respond to the views of stakeholders and to the recommendations of the Independent Reconfiguration Panel.
In developing this SOC discussions have involved engagement with primary and secondary care senior clinicians; external clinical review via NHSE; system meetings with regional leads for NHSI, NHSE and the Integrated Care System; Health & Wellbeing Boards; Joint Health Scrutiny and Local Medical Committees (LMCs). It is planned to continue to fully engage and involve local people, voluntary organisations and key stakeholders in the next steps to deliver the proposed future model for hospital services across Calderdale and Huddersfield.
1.9 Conclusion
This SOC proposes a plan that will improve the quality and safety of hospital services; improve the recruitment and retention of staff; eliminate the Trust’s underlying financial deficit; and deliver economic and affordability benefits compared to continuing with the existing model of hospital care. The West Yorkshire and Harrogate Health and Care Partnership has confirmed the proposals described in this SOC as their highest priority. NHS Improvement and NHS England are requested to support and recommend to the Department of Health and Social Care and the Treasury approval of this SOC.
2. Background & Introuduction
Calderdale and Huddersfield NHS Foundation Trust (CHFT) has two District General Hospital sites, Huddersfield Royal Infirmary (HRI) and Calderdale Royal Hospital (CRH), located 5 miles apart in Huddersfield and Halifax.
There is a compelling quality and financial case for change in the local health and care system. Work to develop a safe and sustainable model of hospital and community care in Calderdale and Huddersfield has been underway since July 2012. Formal public consultation on proposed future arrangements took place during 2016. In September 2017 the Calderdale and Kirklees Joint Health Scrutiny Committee referred the proposals to the previous Secretary of State for Health and Social Care and his recommendations and the advice of the Independent Reconfiguration Panel (IRP) were published in May 2018. This set out that further work focusing on out of hospital care, hospital capacity and the availability of capital funding was required by the NHS before a conclusion could be reached.
During the summer of 2018 significant work was therefore undertaken by local NHS organisations, working with NHS England (NHSE) and NHS Improvement (NHSI) and engaging the Chairs of the Joint Health Scrutiny Committee, Health and Wellbeing Boards, and the Local Medical Committees (LMCs), to develop an enhanced proposal for the future model of care. The enhanced proposal sought to ensure the best possible clinical outcomes for patients within available resources and to address the issues identified by the Independent Reconfiguration Panel (IRP) in its report. An update describing the enhanced proposal (and the stakeholder engagement undertaken that informed this) was sent to the Secretary of State for Health and Social Care in August 2018.
During the summer of 2018 West Yorkshire & Harrogate Health and Care Partnership supported the national capital funding prioritisation process and agreed these proposals as its top priority. The Partnership confirmed that the proposals fit with the overall strategy for the development of better health and care services for West Yorkshire and Harrogate as a whole.
In September 2018 the Secretary of State for Health and Social Care confirmed that he was pleased that rapid progress had been made, with the active involvement of stakeholders, and on 7th December 2018 the Department of Health and Social Care (DHSC) announced that capital funding of £196.5m had been allocated to support implementation of the enhanced proposal. This capital funding allocation was included as part of the Government’s major multi-year £2.9 billion funding package of additional capital investment in the NHS to provide better service models for patients, integrate care services and renew aging facilities.
Following the DHSC announcement of capital funding availability it was also confirmed by DHSC that approval of a Strategic Outline Case (SOC), Outline Business Case (OBC) and Full Business Case (FBC) by NHSI, DHSC, Ministers and HM Treasury would be required. The business cases will be approved by CHFT Trust Board prior to submission to NHSI and letters of support from CCG Governing Bodies, and the West Yorkshire & Harrogate Health and Care Partnership Lead Chief Executive will also be required at each stage of approval. The content of the SOC, OBC and FBC will take account of Her Majesty’s Treasury (HMT) Green Book guidance on appraisal and evaluation and the supplementary Guide to Developing the Project Business Case (2018) and guidance from NHSI.
Based on these requirements and the associated governance processes the table below provides an indicative outline timeline for this development.
| Stage | Submitted to NHSI | NHSI, DHSC, Ministers & HMT Approval |
|---|---|---|
| SOC | April 2019 | December 2019 |
| OBC | February 2020 | October 2020 |
| FBC | January 2022 | September 2022 |
| Commence Build | January 2023 | |
| Complete Build | January 2025 | |
This document therefore provides the Strategic Outline Case (SOC) for the reconfiguration of hospital services in Calderdale and Huddersfield. It describes the plans to improve the safety and sustainability of hospital patient services provided by CHFT, building on the feedback provided by staff, patients, the public and the IRP. The local NHS has worked with the Calderdale and Kirklees Joint Health Scrutiny Committee throughout the development of the plans described. Informal workshops and meetings took place in July and August 2018 and the proposals were discussed at the formal public meeting of the Joint Committee that took place on 7th September 2018. Since then further informal meetings with the Chairs of the Joint Committee were held on 1st October 2018, 5th November 2018 and 22nd January 2019 and a formal public meeting of the Joint Committee was held on 15th February 2019 to further discuss the proposals.
The proposed future model of hospital services in Calderdale and Huddersfield will support and enable delivery of the vision and ambitions described in the NHS Long Term Plan. Digital technology will have a central role in transforming services in order to support more people to have care at, or closer to, home. This will be complemented by a hospital model that provides essential clinical adjacencies and the critical mass required to sustain staff recruitment and retention, ensure quality and deliver revenue savings.
There are a number of areas where the proposed model described in this SOC are unchanged from that which was previously the subject of public consultation (this includes: urgent care; maternity and midwifery services; paediatrics; planned surgery; acute inpatient medical care; critical care; acute and complex surgery, and; outpatient services). Where changes have been made to the proposed future hospital service model this has sought to respond to the views of stakeholders and to the recommendations of the IRP. The key changes are: the continued provision of 24/7 consultant-led A&E services at both sites; the provision of physician-led inpatient care at HRI, and; a commitment to maintain the number of hospital beds broadly as they are now whilst services are developed in the community.
This SOC is structured to explain the proposed service changes from 5 interdependent dimensions – known as the Five Case Model i.e.
| Strategic Case | What is the case for change? What is the current situation? What is to be done? What outcomes are expected? How do these fit with wider government policies and objectives? |
|---|---|
| Economic Case | What is the net value to society (the social value) of the intervention compared to continuing with Business As Usual? What are the risks and their costs, and how are they best managed? Which option reflects the optimal net value to society? |
| Commercial Case | Can a realistic and credible commercial deal be struck? Who will manage which risks? |
| Financial Case | What is the impact of the proposal on the public sector budget in terms of the total cost of both capital and revenue? |
| Management Case | Are there realistic and robust delivery plans? How can the proposal be delivered? |
This SOC describes how the proposed reconfiguration of hospital services enabled by capital investment will:
- Improve the clinical quality of hospital services;
- Improve the efficiency of service delivery and thereby support local and regional system affordability;
- Improve compliance with statutory, regulatory and accepted best practice;
- Make the best use of the available hospital estate.
The Trust recognises the impact of service changes on staff, patients and the public and is committed to working hard to understand and mitigate this impact where possible. The Trust will continue to fully engage and involve staff, local people, campaign groups, key stakeholders and the Joint Health Scrutiny Committee in the next steps to deliver the proposed future model for hospital services across Calderdale and Huddersfield.
3. The Strategic Context
This section provides an overview of the ‘as is’ strategic context for the development of this SOC and provides information in relation to:
- The health needs of people resident in Calderdale and Huddersfield;
- NHS national plans;
- West Yorkshire & Harrogate Health and Care Partnership;
- NHSE Specialised Service Commissioning;
- Calderdale and Greater Huddersfield Clinical Commissioners;
- Calderdale and Kirklees Councils;
- Care Closer to Home;
- Digital Technology
- CHFT current service provision and performance;
- Summary of timeline, key documents and stakeholder engagement previously undertaken.
3.1 Health Needs in Calderdale and Huddersfield
The resident population of Huddersfield and Calderdale is approximately 453,000. People in Calderdale and Greater Huddersfield are living longer lives than in the past, however, more people are likely to have multiple long term conditions and thereby increase the demands on the health and social system. Life expectancy at birth in Calderdale and Kirklees is lower than the England average. As a result, there is a growing population, with more complex health needs, putting more demand on healthcare services in both Calderdale and Huddersfield (see figure 1).
| Figure 1 | Calderdale | Greater Huddersfield |
|---|---|---|
| Population Growth | The population is increasing and will continue to grow, especially in the over 65 and the 0-15 year old age group. It is expected that the population that Calderdale CCG commission services for will increase by 10% over the next 25 years. | The population is increasing and will continue to grow, especially in the over 65 and the 0-15 year old age group. Estimates suggest that by 2030 the population will be 278,700 (an increase of >15.2% since 2010). |
| Mental health and dementia | In Calderdale it is estimated there are 2,300 people living with dementia and this is forecast to increase by about 75% over the next 15 years. | In Kirklees it is estimated there are 4,000 people living with dementia and this is forecast to increase by about 75% over the next 15 years. 1 in 5 adults are reported to be suffering from depression, anxiety or other mental health conditions. |
| Deprivation | Fuel poverty is estimated to affect a quarter of all households in Calderdale. An estimated 1 in 5 children are living in poverty. Higher rates of infant mortality are associated with higher levels of deprivation, and the infant mortality rate (MR) for Calderdale is significantly higher than the England average (7.53 per 1,000 live births compared to 4.69 per 1,000 births). | There are high poverty and deprivation levels in Greater Huddersfield with higher rates of unhealthy behaviours and higher disease burden. Long term pain, depression and anxiety have the largest impact on local health. |
| Lifestyle factors and obesity | Behavioural factors which relate to health are not improving. Smoking prevalence and the harm caused by alcohol and obesity is increasing. There is rising childhood obesity and it is estimated that 40% of all illness in Calderdale can be attributed to lifestyle factors. | Lifestyle choices have a significant impact on the major causes of ill health and premature death in Greater Huddersfield. 53% of adults in the Greater Huddersfield area are overweight or obese, and 1 in 5 children are overweight or obese. |
| Life expectancy and inequalities | More people are living longer with multiple health problems. There is a growing health gap, with those living in Calderdale’s most disadvantaged communities experiencing greater ill health than elsewhere in the district (there is a life expectancy gap within wards within Calderdale of up to 11 years). | More people are living longer with multiple health problems. Life expectancy varies across Greater Huddersfield, with the gap in life expectancy at birth at 3.4 years for men and 3 years for women. |
Preventing avoidable illness (through actions such as smoking cessation, obesity reduction, and lower air pollution) as well as providing better support for patients, carers and volunteers to self-manage long-term health conditions, will be essential to address the health needs of the local population.
3.2 The NHS Long Term Plan
In 2018 the Government announced a £20.5bn annual real terms uplift for the NHS by 2023/24 and in January 2019 the NHS long term plan was published. The Plan describes ambitions over the next ten years to ensure the NHS is fit for the future and details improvements to be delivered in the following key areas:
- Improving out-of-hospital care (primary and community services);
- Strengthening the NHS contribution to prevention and reducing health inequalities;
- Reducing pressure on emergency hospital services;
- Delivering person-centred care;
- Delivering digitally enabled primary and outpatient care;
- Focusing on population health and local partnerships with Integrated Care Systems having
a central role in the delivery of the Plan. The proposed future model of hospital services in Calderdale and Huddersfield described in this SOC will support and enable delivery of the vision and ambitions described in the NHS Long Term Plan. In particular, the NHS Long Term Plan confirms that: "separating urgent from planned services can make it easier for NHS hospitals to run efficient surgical services. Planned services are provided from a ’cold‘ site where capacity can be protected to reduce the risk of operations being postponed at the last minute if more urgent cases come in. Managing complex, urgent care on a separate ’hot‘ site allows trusts to provide improved trauma assessment and better access to specialist care, so that patients have better access to the right expertise at the right time. So we will continue to back hospitals that wish to pursue this model."
3.3 West Yorkshire & Harrogate Health and Care Partnership
Integrated Care Systems (ICSs) will be central to the delivery of the NHS Long Term Plan. They bring together local organisations to redesign care and improve population health, creating shared leadership and action. The West Yorkshire and Harrogate Health and Care Partnership (ICS) is the second largest in the country covering a population of 2.6 million people and a budget of over £5 billion. The purpose of the partnership is to deliver the best possible health and care for everyone living in the areas of: Calderdale; Kirklees; Bradford District and Craven; Leeds; Wakefield; Harrogate. The Partnership is made up of care providers, commissioners, voluntary organisations and Councils working closely together to plan health and care.
During 2018 West Yorkshire and Harrogate Health and Care Partnership supported the national capital funding prioritisation process and agreed the proposals described in this SOC as their top priority confirming that the Partnership was confident that these proposals fit with the overall strategy for the development of better health and care services for West Yorkshire and Harrogate as a whole.
The ICS has supported the developments in Calderdale and Huddersfield throughout the process of developing this SOC in a material and meaningful way:
- All organisations across the partnership made investment in Calderdale and Huddersfield the number one priority for capital bids in the last round. This helped secure funding for the system.
- The ICS has funded additional work to develop the models that will be required to support more people within communities and accelerate the development of local care networks.
- The ICS is playing a lead role in the Local Health Care Record Exemplar (LHCRE) programme, which is both supporting the work within Calderdale and Huddersfield, and learning from the work to inform progress across the whole region.
- The ICS has been fully involved in local scrutiny discussions, as well as political discussions at a local and national level.
A letter of support from the West Yorkshire Health and Care Partnership for this SOC is provided at section 13.
3.4 NHSE Specialised Service Commissioning
NHS England (NHSE) commissions 149 specialised services across England. Specialised services are provided in relatively few hospitals and accessed by comparatively small numbers of patients, but usually with catchment populations of more than one million. CHFT currently provides the following specialised services:
- Vascular surgery and vascular interventional radiology services;
- Neonatal intensive care;
- HIV;
- Chemotherapy;
- Bone anchored hearing aids (BAHA);
- Cardiac MRI;
- Implantable cardiac device.
During 2016/17 NHSE undertook a review of vascular specialised services across Yorkshire and Humber and recommended that West Yorkshire should move from 3 to 2 vascular arterial surgery centres, with one at Leeds due to the major trauma centre and one at either Bradford Teaching Hospitals NHS Foundation Trust (BTHFT) or Calderdale and Huddersfield NHS Foundation Trust. At the request of NHS England, the West Yorkshire Association of Acute Trusts (WYAAT) worked with vascular clinicians from across West Yorkshire to make a recommendation on its preferred option for the future location of arterial centres and in April 2017 the WYAAT Committee in Common (CIC) unanimously agreed to recommend BTHFT as WYAAT’s preferred option to NHS England. NHS England is currently progressing engagement and dialogue to take forward this recommendation. This SOC has been developed on the assumption that CHFT in the future will not provide acute vascular arterial surgery (this means that the development of a hybrid theatre has not been included in the proposed estate development).
3.5 Calderdale and Greater Huddersfield Clinical Commissioners
NHS Calderdale and NHS Greater Huddersfield Clinical Commissioning Groups (CCGs) commission the majority of hospital and community health services for the Calderdale and Greater Huddersfield populations. Both CCGs are progressing plans to improve: the quality and safety of care; outcomes for patients; service affordability and sustainability. The Governing Bodies of Calderdale CCG and Greater Huddersfield CCG have previously agreed that there is a compelling case for changing the way that local health services are provided and that if the local system is unable to redesign and transform services in a way that drives up quality, then patients will experience poorer outcomes as a result.
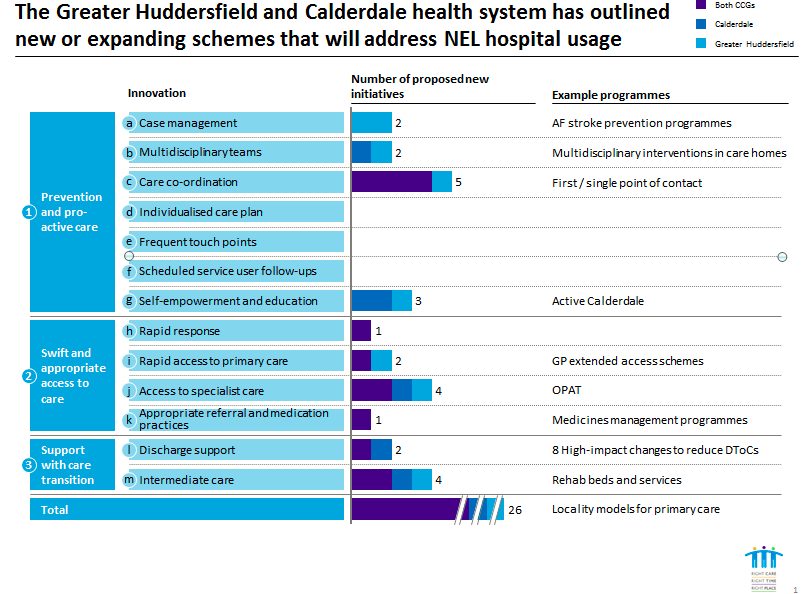
Working closely with Kirklees and Calderdale Health and Wellbeing Boards and local stakeholders, both CCG plans include: the development of care closer to home (described in more detail below); the reconfiguration of hospital services; and the increased use of digital technology.
During 2016 the CCGs led the Right Care, Right Time, Right Place formal public consultation on proposed future arrangements for hospital and community health services in Calderdale and Greater Huddersfield. Since 2016 the CCGs have continued to work closely with Calderdale and Kirklees Joint Health Scrutiny Committee and local stakeholders to respond to the findings of the Public Consultation and to the issues raised by the Independent Reconfiguration Panel. The outputs from this work have informed and are reflected in the proposals described in this SOC.
The CCGs will formally consider this SOC during April to determine whether the proposals described will improve clinical care and outcomes for the Calderdale and Greater Huddersfield population; that the proposals are affordable to Commissioners, and that the proposals will improve and achieve the financial sustainability of the Calderdale and Greater Huddersfield system of care.
Letters of support from Calderdale and Greater Huddersfield CCGs for this SOC are provided at section 13.
3.6 Local Councils and Committees
3.6.1 Calderdale and Kirklees Councils
There has been on-going engagement with Calderdale and Kirklees Councils in relation to the revised proposals described in this SOC. The view of each Council is shown below.
"Calderdale Council has supported the proposals and agreed that they are wholly consistent with the Council’s strategic intent and plans. The Council has confirmed it will take all necessary action to work with the local health system to realise the full impact of the investment and the delivery of a sustainable health and social care system in the future. This work fits with Calderdale’s 2024 Vision and its focus caring for local people as a part of Calderdale Cares."
"Kirklees Council recognises that there are quality, cost and sustainability pressures across the whole health and care system and that change will be required to address this. These pressures face all the healthcare providers that support Kirklees residents and considering only one of these providers will not result in the best solution for Kirklees. The configuration of services delivered by CHFT cannot be considered in isolation from those delivered by Mid Yorkshire Trust which also experiences pressures, has re-configured services but will need to further re-configure including those services currently delivered in Kirklees. The Council believes that the exact configuration of services should be determined through a comprehensive review of all health and social care services and facilities across Kirklees including community provision because we know that a number of our community facilities are not ideal. This process should be supported by a single plan for Kirklees rather than individual organisations planning in isolation from each other. The Council considers that there is scope for operational and financial efficiency if the 2 acute providers that serve Kirklees were to collaborate and work together to re-configure services within Kirklees. This feels to be much more in line with the concept of an ICS than the current approach of organisational silos. Whilst the Council welcomes investment into local health services and recognises that there are some urgent short term estates issues, the Council would not want to see investment in solutions that constrain future change, particularly knowing that the re-configuration proposals made by CHFT are only a short term solution and not a sustainable long term plan. The Council also believes that significant investment is required in prevention, staying well and helping people to manage their own health conditions effectively. This includes investment in community health care services, social care and voluntary sector capacity, all of which have seen significantly less focus and investment than the primary, mental health and acute care sectors. It is helpful to see that the NHS 10 Year Plan recognises this and we welcome the opportunity to work with local commissioners and providers to make this happen"
3.6.2 Calderdale and Kirklees Local Medical Committees
Calderdale Local Medical Committee (LMC) has previously expressed its position that "maintaining the status quo in regards to the configuration of local health services is not an option and that the revised proposals in response to the IRP is well considered and positive".
Kirklees Local Medical Committee (LMC) has advised: "We still believe that a joint and collaborative exercise to devise a more practical solution for the delivery of health, social and community care in our area is necessary and desirable, utilising both Calderdale and Huddersfield’s hospital sites, for the benefit of our populations over at least the next two generations."
3.7 Care Closer to Home
Significant progress has already been made in both Calderdale and Kirklees in the development and delivery of care closer to home.
In Calderdale, as a consequence of strengthened partnership approach operating between the CCG, the Local Authority and CHFT, the system’s performance on Delayed Transfers of Care (DTOC), has moved from being amongst the weakest performing systems nationally to being consistently amongst the best. (Calderdale Local Authority as at January 2019 ranks 21st out of 151 nationally for all delays and 12th out of 151 nationally for NHS only delays.)
Greater Huddersfield CCG is one of seven national Intensive Support Sites, with the intention of increasing GP retention and strengthening the out of hospital workforce. Through this programme, support for practices is developing, for example by increasing the number of training practices in the Kirklees area, and for individual GPs through GP mentorship, coaching and leadership development. This is also supported by wider system initiatives, such as work to understand the impact on workload at the interface between primary and secondary care. These initiatives are in addition to significant investment by NHS England to attract new GPs to practices, including providing more training places and an international recruitment programme.
In both Calderdale and Kirklees, networks of GP practices have been brought together, to serve and design care for ‘localities’ of 30,000-50,000 people, in line with the NHS Long Term Plan. This structure is expected to form the basis of community care and public health service provision within both places providing a place-based framework for Health and Social Care where organisations work together and share resources to deliver holistic person-centred care. The aim is to make it easier for people to access care when closer to home, with a consistent and high quality experience for patients as they move between different parts of the integrated system.
The current plans, and those of the wider system, for out-of-hospital care, could reduce acute hospital bed days by 10% over five years, if they reach their full potential. This would more than absorb the forecast increase in hospital usage from demographic growth.
To significantly improve the care and population health management out of the acute setting, a wider transformation of services is required. Health systems around the world are moving to a model of care outside of the hospital that integrates all primary care, community, mental health and social care services. Best-performing systems fully integrate their services (including nursing, social care and community care) within their localities, co-locating front-line staff within integrated community hubs. This approach enables better co-ordination of care, and better identification and provision of appropriate packages of care to patients according to their individual need. This improved care means people do not have to go to hospital so frequently and once there can leave it more quickly. This delivery model would enable us to deliver all of the components of integrated care systems, tailored as appropriate to the needs of our individual patients.
As care in Calderdale and Kirklees is redesigned around the localities, there is an opportunity to follow best-performing out-of-hospital systems in the UK and worldwide, by designing packages of care around the needs of the population and joining up and co-locating delivery of community, primary and social care services through teams that comprise a range of staff such as GPs, mental health professionals, pharmacists, district nurses, community geriatricians, dementia workers and Allied Health Professionals such as physiotherapists and podiatrists/chiropodists, joined by social care and the voluntary sector.
The West Yorkshire & Harrogate Health and Care Partnership has supported the CCGs to undertake detailed capacity modelling to compare the existing models of care closer to home with examples of best practice and to quantify the future community and primary care workforce and facilities capacity that will be required to achieve an optimal reduction in demand for hospital services. The best of these integrated care systems in both England and internationally have 20-40% fewer non-elective bed days per head of population than Calderdale and Greater Huddersfield CCGs. These systems, starting from a similar baseline, have in a number of cases made these improvements through substantial transformations of their services over 4-6 years.
From the evidence base, set out in detail in the report, the CCGs have set an aspiration to reduce non-elective bed days for the population by 30% over 5 years. This would make Calderdale and Greater Huddersfield CCGs some of the best-performing areas in the UK for this measure. A summary of the report is provided at Annex A.
This modelling will inform future CCG investment decisions in primary and community services to address demand pressures, enable workforce expansion, and develop new services to meet the needs of the population. The total number of hospital beds will continue to remain broadly as they are now whilst these integrated services are developed in the community and demonstrate a sustainable reduction in the demand for in-patient hospital care.
The CCGs will continue to work closely with Kirklees and Calderdale Health and Wellbeing Boards and local stakeholders to progress the plans for development of care closer to home.
3.8 Digital Technology
The development of digital technology in Calderdale and Greater Huddersfield over the last few years has been significant. CHFT is now one of the most digitally advanced Trusts in the country. CHFT in partnership with Bradford Teaching Hospital Trust has successfully implemented the Cerner electronic patient record across well over a third of the population of the West Yorkshire & Harrogate Health and Care Partnership footprint. In addition to this and as a part the West Yorkshire Association of Acute Trusts programme there has been work done on developing a regional imaging collaborative as well as interoperability across laboratory information management systems, some of which involves national genomics testing on behalf of NHSE.
CHFT has some of the highest utility of the national electronic staff record (ESR) and has been successfully using an App (application software) for recruitment of bank staff for several months, as well as leading the way nationally on implementing the K2 Athena maternity patient record and recently the same system went live in Leeds Teaching Hospitals Trust again providing consistency of approach in West Yorkshire.
Working in partnership with commissioners and fellow providers, CHFT has been able to demonstrate progress when measured against NHS England’s Digital Maturity Assessment resulting in a movement to joint third of the 41 groupings in England.
Digital technology is currently enabling clinicians to access and interact with ‘real-time’ patient records and care plans wherever they are. The Trust’s aim is to ensure that staff and patients have access to the right information and data, at the right time, to optimise the delivery of effective, safe, high quality care. To achieve this we are working towards enabling digital systems to talk to each other, so that data can flow seamlessly across health and care settings. During 2018 the Trust has:
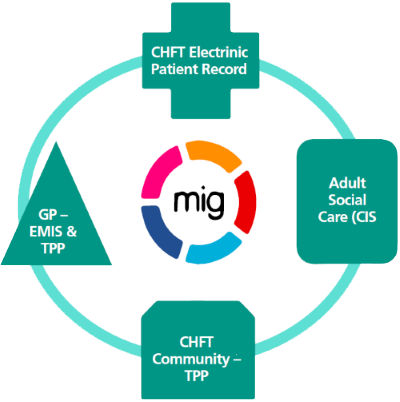
- Used the Cerner Health Information Exchange (HIE) and the Medical Interoperability Gateway (MIG) to enable ‘real-time’ patient information to be shared across GP practices and the hospital. All GPs in Calderdale and Greater Huddersfield can now view the hospital electronic patient record in their system of choice (SystmOne and EMIS) - this is a real time view and not via a separate portal. Hospital clinicians can also now view the GP record for all Calderdale and Greater Huddersfield patients within the hospital Cerner electronic patient record. Calderdale Community Service staff can also view the Calderdale GP record for both SystmOne and EMIS. Work has also commenced to progress digital inter-operability with the Calderdale Social Care System via the MIG. This development will enable integration of the adult health and social care records in the future. The progress being made to connect digital health and care systems is illustrated below;
- Continued to implement the use of digital technology to enable transformation of outpatient services and the provision of virtual clinics that mean patients don’t have to make unnecessary visits to hospital and offer more efficient, convenient and timely access to services;
- Implemented a digital Electrocardiogram (ECG) management system that means ECG carts are now fully integrated with the electronic patient record. This has improved the efficiency of requesting ECGs and enabled the immediate availability of digital ECG test results for clinical review. This is enabling more timely clinical decision making and subsequent treatment and intervention to support patient care;
- Implemented digital blood tracking system (Haemonetics) that means all blood products are barcoded and identifiable. This system will improve safety and efficiency and in the future will enable the safe remote vending of blood products across the two hospital sites.
Work in Calderdale and Greater Huddersfield is also being progressed to develop digital health solutions such as telecare, telehealth tele-monitoring and direct booking of appointments from 111 to GPs.
These local developments in the use of digital technology are fully aligned with and support the work of the Yorkshire & Humber Local Health and Care Record Exemplar (LHCRE) project. The aim of the LHCRE project is to join up clinical systems across the region to support integrated care and to empower patients to take control of their condition by providing access to their own healthcare records. The Trust will work with NHSX to progress implementation of local digital innovation and developments to improve health and social care.
3.9 Calderdale and Huddersfield NHS Foundation Trust
Calderdale and Huddersfield NHS Foundation Trust (CHFT) is an integrated Trust that provides acute and community health services. The Trust serves two populations; Greater Huddersfield which has a population of 248,000 people and Calderdale with a population of 205,300 people. The Trust operates acute services from two main hospitals; Calderdale Royal Hospital (CRH) and Huddersfield Royal Infirmary (HRI). The distance between the two hospitals is 5 miles. The Trust also provides community services in the Calderdale area. The Trust has approximately 800 beds, and 6,000 staff and an annual planned operating expenditure in 2019/20 of £408m.
HRI is an aging 1960s District General Hospital (DGH) with significant estates maintenance challenges and the Trust carries a very high risk in terms of the condition and reliability of its buildings at HRI. The age and condition of the estate means that some buildings are not clinically fit for purpose and without a significant capital injection there is a very high risk of failure of critical estate services and consequent impact on service delivery. An updated 6 Facet Estate Survey is currently being undertaken to assess the condition and reliability of the buildings and the engineering services infrastructure at HRI.
CRH opened in 2001. It was built using PFI funding and remains a DGH suitable for modern models of healthcare provision. Acre Mills, adjacent to HRI, is a modern base for out-patient appointments, and opened in February 2015.
Both hospitals currently provide accident and emergency services, outpatient and day-case services, acute inpatient medical services and intensive care for adults. Some services are delivered at one site only (e.g. stroke, trauma, and maternity services). For a number of years CHFT has experienced clinical, operational and financial challenges associated with the dual site provision of services.
Nationally there has been a rapid rise in the demand for hospital nurses and other health professionals, and difficulties in recruiting consultants in several specialties. Growing shortages of qualified clinical staff has increased use of agency and other temporary workers to fill vacancies, and this has increased NHS expenditure and made services less stable. This national workforce pressure is further amplified at CHFT due to the dual site configuration of most services which makes it difficult to recruit and retain staff and has resulted in a reliance on temporary and agency staffing to sustain service delivery.
The aim of the Trust’s workforce strategy is to ‘ensure a workforce of the right shape and size with the commitment, capability and capacity to deliver safe, efficient, high quality patient care’. A key enabler for this will be the reconfiguration of hospital services to reduce dual site working.
The Trust has a significant financial deficit and is reliant on loans and funding support from the Department of Health and Social Care. Structural costs associated with the dual site configuration of services (which requires higher workforce expenditure) is a key factor driving the Trust’s underlying deficit.
Over the last two years across the combined and ranked metrics of Referral to Treatment Times (RTT), Emergency Care Standard (ECS) and Cancer waiting time less than 62 Days, CHFT has consistently been one of the best performing Trusts in England.

In 2018 CHFT was inspected by the CQC and received an overall rating of “Good” for the services it provides and “Requires Improvement” for the Use of Resources. The CQC assessment commented that “The trust recognises that its current configuration of two acute sites is not financially sustainable. Operationally this places limitations on the trust’s ability to make best use of resources” and “The trust has a very strong model of CIP (cost improvement planning) governance arrangements in its systems and processes which have been promoted as an exemplar for others to adopt”.
Maintaining good standards of performance at CHFT is fragile as it is reliant on the continued use of temporary and agency staff and the costs associated with this. Nationally standards are also being raised, including the expectation that services are offered 7 days a week. These changes will lead to better outcomes – people living longer and healthier lives – but they present a challenge in trying to deliver a comprehensive set of services across the current two site configuration, at sufficient scale to meet standards 7 days a week.
The Trust’s Vision – “Together we will deliver outstanding compassionate care to the communities we serve” – provides the context for the current and proposed future clinical and operating models described in this SOC.
This vision is underpinned by four fundamental behaviours that guide all Trust employees in the way they work.
3.10 Timeline of Previous Work and Stakeholder Engagement
| 2013 |
|
|---|---|
| 2014 |
|
| 2014 |
|
| 2014 |
|
| 2015 |
|
| 2015 |
|
| 2016 |
|
| 2017 |
|
| 2018 |
|
3.11 Key Documents Previously Published
• National Clinical Advisory Team (NCAT) Report - Calderdale and Huddersfield NHS Foundation Trust Accident and Emergency Services (2013)
• Call to Action: Engagement Report for Calderdale and Huddersfield Strategic Review (2014)
• Right Care, Right Time, Right Place - Strategic Outline Case - Transforming Services in Greater Huddersfield and Calderdale (2014)
• Right Care, Right Time, Right Place - Outline Business Case - Transforming Services in Greater Huddersfield and Calderdale (2014)
• People’s Commission Calderdale Council (2015)
• Hospital Services Potential Outline Future Model Of Care - Clinical Consensus Model (2015)
• Yorkshire and the Humber Clinical Senate Review of the Future Model of Hospital Services for Calderdale and Greater Huddersfield CCGs (2015)
• Calderdale and Huddersfield NHS Foundation Trust (CHFT) implementation of the potential outline future model of care for hospital services: Quality Impact Assessment (2015)
• 5 Year Strategic Plan for Calderdale and Huddersfield NHS Foundation Trust (2016)
• Right Care, Right Time, Right Place - Pre-Consultation Business Case (2016)
• Right Care, Right Time, Right Place - Public Consultation On Proposed Future Arrangements for Hospital and Community Health Services (2016)
• Independent Report of the Findings of the Right Care, Right Time, Right Place Public Consultation (2016)
• Equality & Health Inequality Impact Assessment - Right Care, Right Time, Right Place (2016)
• Reconfiguration of Calderdale and Huddersfield NHS Foundation Trust - Full Business Case (2017)
• Calderdale and Kirklees Joint Heath Scrutiny Committee Referral of Proposed future arrangements for hospital and community health services in Calderdale and Greater Huddersfield to the Secretary of State for Health (2017)
• Right, Care Right Time, Right Place - Calderdale and Greater Huddersfield Travel and Transport Review - Report of the Independent Chair (2018)
• Advice of the Independent Reconfiguration Panel On The Right Care, Right Time, Right Place – Proposed Future Arrangements for Hospital and Community Health Services In Calderdale and Greater Huddersfield (2018)
• NHS Progress Reports submitted to the Secretary of State for Health and Social Care in August 2018 and January 2019
• Letter of clinical advice from Dr David Black – Medical Director (Joint) – North Region (Yorkshire and the Humber) and Deputy National Medical Director Specialised Commissioning NHSE (2018)
4. The Case For Change
There is a compelling quality, workforce, estates and financial case for change in the local health system.
4.1 Quality
For people that have a serious life-threatening illness or injury and need emergency services it is not currently possible to guarantee the consistent presence of senior doctors seven days a week. The Trust is experiencing the effects of a national shortage of emergency doctors at both consultant and middle grade levels. The current consultant pool is stretched covering vacancies which the Trust is unable to recruit to. As a result, the two emergency departments are heavily reliant on cover from locum middle grade doctors.
The two emergency departments at Calderdale Royal Hospital (CRH) and Huddersfield Royal Infirmary (HRI) are non-compliant with many of the standards for Children and Young People in Emergency Care settings with regards to having ready access to paediatric specialist trained staff. Paediatric medicine and surgery are not co-located on the same hospital site and this means that for children who have urgent medical and surgical needs there are challenges in providing shared care from a consultant surgeon and a paediatrician.
There is often a need for transfer of patients between sites due to not all the expertise needed to manage certain conditions being co-located. Also, for people with multiple medical problems when they are admitted to hospital, too many people experience a number of moves between wards, a longer length of stay in hospital, and increased risk of a poor experience and outcomes.
Some planned operations are cancelled at short notice because staff and facilities are needed to respond to meet the needs of emergency patients.
Without change too many people will:
- Be admitted to residential or nursing home care;
- Stay longer in hospital than is clinically necessary (which can be a factor which contributes to deteriorating health);
- Be admitted to hospital with a long term condition;
- Be readmitted within 30 days;
- Report that they do not have a good experience when they attend A&E and leave A&E without having been seen;
- Have their planned operations cancelled to release staff and facilities to meet the needs of emergency patients;
- Need to be moved between the two hospitals increasing the risk of a poor experience and outcomes.
4.2 Workforce
The Trust faces considerable workforce challenges which undermine the resilience of clinical services, staff satisfaction and wellbeing, and the Trust’s finances, this includes:
- Non-compliance with Royal College of Emergency Medicine workforce recommendations and the standards for Children and Young People in Emergency Care settings with regards to having ready access to paediatric specialist trained staff;
- Non-compliance with Guidelines for the Provision of Intensive Care Services 2015 (GPICS) standards as consultants have other areas of responsibility when on call;
- Intense and fragile clinical rotas;
- Recruitment and retention challenges resulting in a heavy reliance on locum and agency staff (and additional expenditure of circa £14m per annum).
These challenges are largely due to the current dual-site service model as well as national workforce shortages. As a result the Trust is not able to substantively recruit to meet the medical rotas of the two sites, and a number of recruitment processes have failed due to lack of applicants.
Consultant staff have chosen to leave the Trust in Emergency Medicine, Radiology and other Medical specialties. The reason given for this is the current configuration of Trust services across two sites. This compromises the quality of care that can be provided, and impacts on workload and frequency of on-call responsibilities.
Dual site running, particularly in relation to out of hours rotas, is increasing the reliance on junior and/or temporary staff. The reliance on middle grade doctors results in less timely specialist input into patient care. The widespread use of locums / temporary staff can also result in a lack of continuity of care, and a negative impact on staff morale and sickness absence rates.
The following specialties are examples of where the Trust is currently experiencing significant recruitment and retention challenges; Emergency Medicine, Gastroenterology, Urology, Radiology, Dermatology, Rheumatology, Ophthalmology, Critical Care, and Acute Medicine.
4.3 Estates
Huddersfield Royal Infirmary (HRI) is an aging 1960s District General Hospital (DGH) with significant estates maintenance challenges and the Trust carries a very high risk in terms of the condition and reliability of its buildings at HRI. The age and condition of the estate means that some buildings are not clinically fit for purpose and without a significant capital injection there is a very high risk of failure of critical estate services and consequent impact on service delivery. An updated 6 Facet Estate Survey is currently being undertaken to assess the condition and reliability of the buildings and the engineering services infrastructure at HRI. This will inform future priorities for investment and is likely to include: upgrade of A&E resuscitation, upgrade of ward areas, replacement of windows, stone cladding, air handling, pipe work, fire safety, drains and asbestos removal.
4.4. Finances
The Trust’s forecast year-end financial position for 2018/19 is delivery of the position at the planned level, a deficit of £43.1m. Securing this position has been challenging in requiring delivery of a Cost Improvement Programme (CIP) of £18.0m, of which the full year effect carried forwards into 2019/20 stands at 86%. Transformational savings programmes and cross system working have been enabled by an Aligned Incentive Contract agreed with the Trust’s two main commissioners, Greater Huddersfield CCG and Calderdale CCG. This successful approach to contracting will continue in 2019/20. In year pressures have been contained through a recovery programme and reinforcing budget holder accountability which will lay a strong foundation for 2019/20. In this context the Trust has confirmed its acceptance of the 2019/20 Control Total of £37.9m. Taking into account the Marginal Rate Emergency Tariff (MRET) allocation at £6.1m, Provider Sustainability Funding (PSF) of £7.3m and Financial Recovery Fund access at £14.8m, the Trust will plan for an overall deficit of £9.7m in 2019/20.
Delivery of this expectation will be stretching from a financial perspective and require implementing transformational change, a focus on budgetary accountability and taking full
advantage of efficiency opportunities to deliver CIP of £11.0m (3%).
The local NHS cannot continue to spend above the funding allocated to it and an efficient model of service delivery is required to ensure that the quality and safety of services are protected whilst spending is brought back into balance. CHFT has significant structural deficits. The proposals described in this SOC will eliminate CHFT’s underlying deficit and thereby will support the financial sustainability of the West Yorkshire and Harrogate Health and Care Partnership.
4.5 External Review Findings and Recommendations
A number of independent reviews and inspections of services have recognised the operational, quality, and workforce challenges described above. This includes: the National Clinical Advisory Team; the Calderdale Council People’s Commission; the Royal College of Physicians; Yorkshire and Humber Clinical Senate; NHS England; NHS Improvement; the Independent Reconfiguration Panel, the West Yorkshire and Harrogate Health and Care Partnership, and; the Calderdale and Kirklees Joint Health Scrutiny Committee. All of these independent reviews have recommended that the status quo i.e. to do nothing is not an option and that changes to the configuration of services are needed to improve outcomes and safety.
- The National Clinical Advisory Team (NCAT) recommended that ‘a one acute care site option was the best for the future safety, value and sustainability of health care’.
- The Yorkshire and Humber Clinical Senate confirmed ‘that a clear argument is made that the current configuration of services does not and cannot meet national guidance and that staying the same is not an option’.
- Calderdale and Kirklees Joint Health Scrutiny Committee have confirmed ‘the Committee accepts that the status quo is not an option and wishes to see improvements in the quality of services provided through hospitals, care closer to home provision and primary care’.
- NHS Improvement and NHS England Regional Directors for the North of England have confirmed that the ‘status quo is not sustainable and the health economy will need to reconfigure to ensure clinical and financial sustainability’.
- The Independent Reconfiguration Panel (IRP) confirmed that ‘maintaining the status quo is not an option’ and that ‘it is only reasonable to continue to pursue the proposals in more detail in the interests of local health services’. The IRP also commented that there was "real concern and a sense of urgency as it has becomes increasingly difficult to recruit and retain key medical staff stretched across two sites".
- The West Yorkshire & Harrogate Health and Care Partnership has agreed the proposals for reconfiguration as their top priority confirming that the Partnership is confident this will support the overall strategy for the development of better health and care services for West Yorkshire and Harrogate as a whole.
4.6 Alignment with NHS Long Term
The proposals for service reconfiguration described in this SOC fully align with the NHS Long Term Plan published in January 2019 which states:
"separating urgent from planned services can make it easier for NHS hospitals to run efficient surgical services. Planned services are provided from a ’cold‘ site where capacity can be protected to reduce the risk of operations being postponed at the last minute if more urgent cases come in. Managing complex, urgent care on a separate ’hot‘ site allows trusts to provide improved trauma assessment and better access to specialist care, so that patients have better access to the right expertise at the right time. So we will continue to back hospitals that wish to pursue this model."
4.7 Clinical Support
Senior doctors, nurses and therapists that currently provide the services in hospital and in the community have identified the need for service and system change to improve the safety and effectiveness of care for patients in the future. Over a number of years clinical colleagues across primary, community, ambulance, social care and hospital services have been engaged and the proposals described in this SOC reflect their views and a wide body of clinical support for the changes proposed.
4.8 Constraints, Dependencies and Risks
Based on the information that has already been described in relation to the strategic context (chapter 3) and the case for change, a number of high level project constraints, dependencies and risks have been identified. These are summarised below and have been taken into account in the subsequent chapters of this business case.
4.8.1 Constraints
- The Trust must make best use of its estate including the full utilisation of the existing CRH PFI estate.
- The preferred funding source is 100% Public Dividend Capital (there is no agreement to private finance initiatives).
- The capital cost of the scheme must not exceed £196.6m.
- The clinical service model must be consistent with the model described in reports submitted to the Secretary of State for Health and Social Care in August 2018 and January 2019. (This model incorporates changes that respond to the recommendations of the Independent Reconfiguration Panel).
- The proposed service changes must be affordable to Commissioners and to the wider system.
- The proposed service changes must improve efficiency and enable the Trust to eliminate its financial deficit.
4.8.2 Dependencies
- Progression of the project is dependent on the Trust maintaining the strategic support of the West Yorkshire and Harrogate Health and Care Partnership and support from Calderdale and Greater Huddersfield CCGs.
- Realising the optimal benefits from this project will be dependent on the use of digital technology to enable interoperability across primary. social care and secondary care systems (see section 3.8).
- The project is dependent on the agreement of clinical protocols with Yorkshire Ambulance Services to ensure patients are transported to the hospital that provides the services that will meet their clinical needs – whether this is in Halifax, Huddersfield or other specialist providers, such as Leeds.
- The project is dependent on the Trust securing necessary agreements with the existing PFI provider regarding the interface of the existing PFI buildings and site for the development of new build at CRH.
- The project will require agreement with other local Trusts where there may be impact on the numbers of patients attending A&E services.
- The project is dependent on effective on-going public and stakeholder involvement and engagement.
- The project is dependent on effective on-going consultation with the Calderdale and Kirklees Joint Health Scrutiny Committee.
4.8.3 Risks
- The Trust carries a very high risk in terms of the condition and reliability of buildings at HRI. An updated 6 Facet Estate Survey is being undertaken to assess the condition and reliability of the buildings and the engineering services infrastructure at HRI. The findings from this could impact on the timing of investments required at the HRI site.
- The Programme Board will ensure that robust arrangements for the on-going management of risk during the key phases of the programme are established. A list of the likely areas of risk management that will be included on the programme risk register is provided at section 11.3.
4.9 Conclusion of the Case for Change
NHS services within Calderdale and Huddersfield face an increasing challenge of delivering high quality, safe and sustainable services. This is within a climate of rising demand and significant workforce recruitment and capacity challenges. These challenges and their potential solutions have been debated for a number of years in Calderdale and Huddersfield and whilst day to day operational plans are in place to ensure the care and safety of patients within the Trust’s clinical services, a sustainable solution is urgently needed.
5. Proposed Service Model
5.1 Hospital Services
The proposed future model of hospital services in Calderdale and Greater Huddersfield will support and enable delivery of the vision and ambitions described in the NHS Long Term Plan. Digital technology will have a central role in transforming services supporting more people to have care at, or closer to home complemented by a hospital model that provides essential clinical adjacencies and the critical mass required to sustain staff recruitment and retention, ensure quality and deliver revenue savings.
The proposed model will make use of both existing hospitals. Both sites will provide 24/7 A&E services and a range of day-case, outpatient and diagnostic services - although where possible services will be delivered in the community and closer to people’s homes. The total number of hospital beds will remain broadly as they are now whilst services are developed in the community and demonstrate a sustainable reduction in the demand for in-patient hospital care. Digital Health capability such as the electronic patient record and patient portals will enable ‘real-time’ review and advice on patient’s care to be provided by specialist staff where required.
Tertiary services will continue as now to be provided in Leeds and at other specialised service providers.
5.2 The Detailed Hospital Services Plan
- Huddersfield Royal Infirmary (HRI) and Calderdale Royal Hospital (CRH) will both provide 24/7 consultant-led A&E services. As is the case now this will mean a 24/7 presence of middle grade Emergency Doctors on each site and Consultant staff on-site for a proportion of each day with 24/7 on call responsibility.
- The A&E at CRH will receive all blue light emergency ambulances for patients that have serious life-threatening conditions and all patients likely to require hospital admission following triage by the Yorkshire Ambulance Service (YAS). The A&E at HRI will receive self-presenting patients. All patients requiring acute inpatient admission will be transferred by ambulance from HRI to CRH. Digital technology will ensure that specialist advice will always be available across both sites, therefore creating more service resilience and enhancing patient safety.
- CRH and HRI will both provide medically led 24/7 urgent care and will be able to treat children 5 years and older with minor illness or injuries and those children considered to have minor illness after triage by 111. Children, who are more seriously ill, have serious injury or are under 5 years old will be quickly triaged, stabilised and if necessary, transported to CRH. Paediatric emergency care and all inpatient paediatric services will be provided at CRH.
- 24/7 anaesthetic cover will be provided at HRI to enable the safe delivery of accident and emergency services. As is the case now this this will mean a 24/7 presence of middle grade Anaesthetists, and Consultant staff on-site for a proportion of each day with 24/7 on call responsibility.
- Critical care services, emergency surgical and paediatric surgical services will be provided at CRH;
- Physician-led inpatient care will be provided at HRI. This is for people who do not require the most acute clinical inpatient healthcare but do require extra support whilst arrangements are made to meet their future needs;
- The total number of hospital beds will remain broadly as they are now whilst services are developed in the community and demonstrate a sustainable reduction in the demand for in-patient hospital care.
- Extended ante-natal, intra partum and post-natal care will be provided in the community where possible and choice will be offered in relation to where the birth takes place. Midwifery led maternity services will be provided on both hospital sites. Consultant led obstetrics and neo-natal care will be provided at CRH.
- Planned surgery and care will be provided at HRI. Patients that require complex surgery or it is known that they will require critical care after surgery will be treated at CRH.
An overview of the proposed service configuration is shown below:

Huddersfield Royal Infirmary
- 24/7 A&E and clinical decision unit
- 24/7 urgent care centre
- 24/7 anaesthetic cover
- diagnostics
- planned medical & surgical procedures
- outpatient services and therapies
- midwifery-led maternity unit
- physician-led step-down inpatient care.

Calderdale Royal Hospital
- 24/7 A&E and clinical decision unit
- paediatric emergency centre
- 24/7 urgent care centre
- 24/7 anaesthetic cover
- diagnostics
- critical care unit
- inpatient paediatrics (medical and surgical care)
- outpatient services and therapies
- obstetrics & midwifery led maternity care
- acute inpatient medical admissions and care (e.g. respiratory, stroke, cardiology).
- acute emergency and complex surgery services
The proposed model will sustainably address quality, operational and workforce challenges and deliver a number of expected benefits that include:
- Local access to urgent and A&E services at both hospital sites;
- Maintaining the total number of hospital beds broadly as they are now whilst services are developed in the community and demonstrate a sustainable reduction in the demand for in-patient hospital care;
- Ensuring paediatric medicine and surgery are co-located on one site facilitating the provision of shared senior paediatric and surgical care for children and young people. This will enable the Royal College standards for Children and Young people in Emergency Care settings to be met.
- A single critical care unit will enable consolidation of the specialist medical and nursing critical care workforce and improve outcomes for patients by ensuring timely senior decision making.
- The reconfiguration of acute inpatient medicine onto one site will reduce the need for the transfer of acutely unwell inpatients across sites. This will improve the safety, experience and outcomes of care.
- The provision of planned surgery and medical procedures at one site will support improved access and reduce waiting times for planned treatment and surgery by minimising the risk of disruption from emergency admissions.
- Consolidation of all blue light ambulance attendances will enable the Trust to improve patient access to the right clinical expertise and better meet the Royal College of Emergency Medicine workforce recommendations. This will improve the likelihood of survival and a good recovery for patients that have life-threatening conditions.
- The realignment of services across the two sites will enable the Trust to deploy staff more efficiently and support meeting standards around 7-day working in the future and the ability to provide specialty rotas. In turn, this will reduce workload pressures on staff and impact favourably on the Trust’s ability to recruit and retain staff reducing the current reliance on temporary staffing.
5.3 Community Services
Many people have said they would wish to be cared for in their own home rather than be admitted to hospital. We also know that for many people their outcomes are often better if they can avoid an unnecessary admission to hospital.
As described in section 3.7, in both Calderdale and Kirklees, integrated community and primary care services are being developed to meet the different levels of need of the local populations. Community based services will be led by multidisciplinary teams of health and care professionals, working together to meet the needs of people who have short-term health needs, individuals with long term conditions and those requiring specialist care for severe or complex needs.
These services will be delivered to populations of 30,000 to 50,000 people in a way that makes it easier for people to access care when closer to home, with a consistent and high quality experience for patients as they move between different parts of the integrated system.
This SOC is based on the commitment that the hospital bed capacity in Calderdale and Huddersfield will remain broadly as it is now whilst services are developed in the community and until it can fully be demonstrated that there has been a sustainable reduction in the demand for in-patient hospital care. This approach is in keeping with the commitment made in the NHS Long Term Plan which states:
"the balance of need for hospital beds will be a product of continuing pressures from an ageing population partially balanced against further gains from changing the model of care. We have not built-in as a core assumption potential offsets in hospital beds from increased investment in community health and primary care. Instead we have provided both for the hospital funding and the staffing as if trends over the past three years continue. So to the extent that local areas are able to do better than recent emergency hospitalisation trends that will deliver for them an additional local financial, hospital capacity and staffing upside dividend."
5.4 Digital Technology
As described in section 3.8, the development of digital technology in Calderdale and Huddersfield over the last few years has been significant which means CHFT is now one of the most digitally advanced Trusts in the country. Digital technology is currently enabling clinicians to access and interact with ‘real-time’ patient records and care plans wherever they are. The Trust’s aim is to ensure that staff and patients have access to the right information and data, at the right time, to optimise the delivery of effective, safe, high quality care. To achieve this, the Trust is working with partners towards enabling digital systems to talk to each other, so that data can flow seamlessly across health and care settings.
Digital technology is a key enabler that will amplify and transmit the benefits associated with the service reconfiguration changes described in this SOC. The changes to service configuration will ensure the Trust has robust clinical service adjacencies and digital technology will support optimising the benefits from this. For services that are provided on a separate hospital site or in the community digital technology will ensure access to “real-time” clinical information and advice. This includes digital inter-operability and multiple access capability across GP, hospital, social care, mental health and community records.
5.5 Quality and Equality Impact Assessment
Prior to public consultation in 2016, an Equality Analysis Report was completed in relation to the protected groups likely to be affected by the proposals; the communities it would be important to reach, and; the variety of formats required to ensure the consultation document was accessible. Post consultation, additional dedicated expert support from the Midlands and Lancashire Commissioning Support Unit was secured to deliver a comprehensive equality and health inequalities impact assessment of the proposals for the consolidation of planned and unplanned hospital services as described in the “Right Care Right Time Right Place” proposals. This concluded that:
- There was no indication of differential impact that would lead to unlawful discrimination linked to the proposals;
- The proposals set out health services to address the needs of the whole population, including those who currently experience disadvantage and the plans are intended to help improve access, experience and outcomes for all;
- The model proposed could have a significant impact on health inequalities for adults, children and young people and those who experience disadvantage by ensuring improved access to more services in the community. This should lead to an improvement in the management of conditions, prevent more extreme intervention being needed and reduce waiting times for urgent care, emergency and acute services.
This SOC builds on feedback from staff, patients, the public and the advice from the Independent Reconfiguration Panel (IRP). There are a number of areas where the proposed model described in this SOC are unchanged from that which was previously the subject of public consultation and an equality and health inequality impact assessment (they include: urgent care; maternity and midwifery services; paediatrics; planned surgery; acute inpatient medical care; critical care; acute and complex surgery, and; outpatient services). Where changes have been made to the proposed future hospital service model, they have sought to respond to the views of stakeholders and to the recommendations of the IRP. The key changes are: the continued provision of 24/7 consultant-led A&E services at both sites; the provision of physician-led inpatient care at HRI, and; a commitment to maintain the number of hospital beds broadly as they are now whilst services are developed in the community.
In July 2018 CHFT therefore undertook further quality and equality impact assessment of the changes that had been made to the proposed model. The findings were presented to CHFT Quality Committee on the 20th July 2018 and to the Board of Directors on the 2nd August 2018. The conclusion of this assessment was that the proposed changes do not generate differential discriminatory equality or health inequality impacts.
5.6 Data Protection Impact Assessment
Section 3.8 described how the Trust is developing the use of digital technology, and that this will support and amplify the benefits of the proposed service reconfiguration. As the proposals are further developed the Trust will consider whether there is the need to undertake a Data Protection Impact Assessment (DPIA).
5.7 NHS England Independent Clinical Advice
During July 2018 NHS Improvement asked NHS England to arrange for independent clinical advice to be given on the proposed clinical model. The NHS England Medical Director for the North Region (Yorkshire and the Humber) arranged for this to be provided by an independent team of eleven clinical colleagues (this included specialists in emergency medicine, acute medicine, mental health, primary and community services). The advice and conclusions of the review confirmed support for the proposed model.
6. Capacity Impact Of The Proposed Model
The Trust has previously been supported by a Senior Economist and an Intelligence Analyst at NHSI to undertake very detailed long-term activity capacity modelling work. This modelling was based on extensive engagement and involvement of clinical colleagues in the Trust across every specialty to review the planning assumptions that were used. For this SOC a high level review and refresh of the previous work has been undertaken. The Trust and commissioners are aligned on the modelling of activity. Further detailed activity and capacity modelling will be undertaken in the development of the Outline Business Case following approval of this SOC.
6.1 Activity Growth Assumptions
The approach taken jointly between CHFT and both Calderdale and Greater Huddersfield CCGs to determine activity growth was based on review of 3-year activity trends.
The 3-year trend analysis initially suggested the following:
- Flat growth for day case, elective and outpatient activity;
- 2% growth for A&E;
- A 5% growth in non-elective short-stay admissions and a 2% growth in non-elective longstay admissions (net growth of 3.8% across all non-elective admissions).
Within this, consideration was then given to the shift seen into ambulatory pathways which had driven a higher growth in emergency short-stay admissions over the past 2-years which is not expected to continue at that same high level. The following growth levels were jointly agreed:
- Flat growth for day case, elective and outpatient activity;
- 2% growth for A&E;
- A 4% growth in non-elective short-stay admissions and a 1% growth in non-elective longstay admissions (net growth of 2.7% across all non-elective admissions);
- 2% growth in community.
This was jointly agreed at point of delivery level and not based upon individual specialty level growth assessments – however, it should be noted that Obstetric and Midwifery non-elective admissions were excluded from this as this had been reviewed separately based on birth rates and known booking rates.
The proposed service changes described in this SOC mean that all blue light ambulance attendances and acute admissions will be diverted to the CRH site. Further work will need to be taken undertaken (subsequent to approval to progress this SOC) that will be informed by discussion with Yorkshire Ambulance Service regarding clinical protocols for ambulance diverts and this will inform future modelling of the volume of A&E and urgent care activity on each hospital site.
6.2 Bed Capacity Assumptions
The Trust currently has potential estate capacity for a total of circa 870 inpatient beds (420 at HRI and 450 at CRH). The Trust manages the number of beds open during the year dependent on patient demand and this is illustrated in the chart below that shows the variation in number of beds open during the previous year.
As at December 2018 the Trust had 806 beds open across HRI and CRH and the average number of beds open during the past 12 months (Dec 2017 – Dec 2018) was 838 beds.
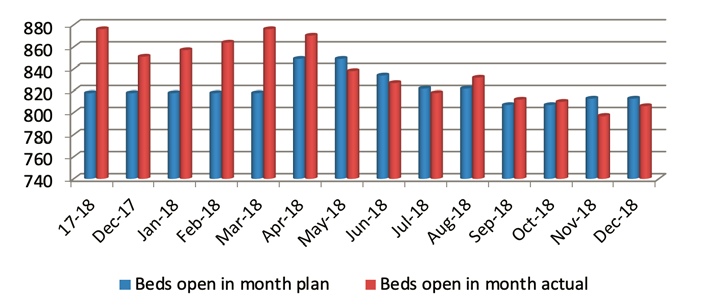
This SOC is based on the commitment that the Trust will continue to provide broadly the same bed capacity whilst services are developed in the community and demonstrate a sustainable reduction in the demand for in-patient hospital care.
Based on modelling previously undertaken in 2017 it is anticipated that the proposed hospital model will require circa 676 acute inpatient beds at CRH and therefore to maintain the total bed capacity broadly as it is now (on average 838) means that circa 162 inpatient beds will be required at HRI for planned care and step-down medical care. A detailed review and updated modelling of bed requirements on each site will be undertaken during development of the Outline Business Case.
As described in section 3.7, the CCGs, supported by the West Yorkshire and Harrogate Health and Care Partnership, have undertaken modelling work that has demonstrated the current plans, and those of the wider system, for out-of-hospital care, could reduce acute hospital bed days by 10% over five years, if they reach their full potential. This would more than absorb the forecast increase in hospital usage from demographic growth. In addition improved efficiency of the delivery of care within the hospital enabled by the use of technology and service reconfiguration (e.g. reducing duplication, transfer of patients between hospitals and delays in accessing specialist advice and diagnostics) will also further mitigate the impact of demographic growth.
6.3 Theatre Capacity
The future theatre capacity requirement is for 8 theatres at HRI and 11 at CRH. This is a growth of one theatre compared to the current 18 provided across HRI and CRH. This is based on elective theatres operating two four hour sessions per day, 5 days per week over 49 weeks. This theatre capacity includes a dedicated 24 hour emergency theatre, a trauma theatre and one emergency obstetrics and gynaecology theatre.
6.4 Impact on other providers
6.4.1 Other Hospitals
Yorkshire Ambulance Service (YAS) and the CCGs have previously calculated patient travel times to both the Calderdale and Huddersfield A&E sites and to neighbouring emergency care providers based on patient postcodes. This modelling showed that the potential impact of CRH being the hospital site for blue light admissions could lead to some patients being diverted and subsequently admitted to a neighbouring emergency care provider (where their ambulance travel time to an alternate provider is less than the travel time to CRH). The impact of this was calculated in 2016 as equating to a total of circa 15 additional beds being required across neighbouring Trusts. This information has previously been shared with all the hospitals affected and the West Yorkshire Association of Acute Trusts.
During 2018/19 service changes that have been implemented by Mid-Yorkshire Hospitals Trust at Dewsbury General Hospital A&E have resulted in some patients from North Kirklees attending the HRI A&E department instead and subsequently being admitted for inpatient care at HRI. This has generated an additional 18 bed capacity requirement at HRI.
Following agreement of this SOC, more detailed work will be undertaken, working with YAS and the West Yorkshire Association of Acute Trusts, to update the modelling assumptions of the anticipated number of ambulance attendances at A&E sites and how this may change as a result of the proposed service model at CHFT and other relevant service changes at neighbouring Trusts.
6.4.2 Yorkshire Ambulance Service
In 2017 Greater Huddersfield CCG and Calderdale CCG commissioned an independent review of the impact of proposed changes in the configuration of hospital services on ambulance services (this updated work previously undertaken in 2015).
The analysis used patient transport data extracted from the Yorkshire Ambulance Service transport management system, covering both emergency calls where a patient is taken to a hospital Emergency Department and the Patient Transport Service (PTS) where patients are taken home from a hospital Emergency Department.
The analysis identified that the impact of the proposal for ‘blue light’ ambulances to travel to the emergency department at Calderdale Royal Hospital would generate requirement for 5,300 hours of additional ambulance time availability per annum.
A further update of this analysis will be undertaken during development of the Outline Business Case and will take account of known changes in demographic demand, changes as a result of the enhanced proposals and any service changes that may have been implemented by the Yorkshire Ambulance Service and at surrounding hospitals since 2017 that could impact on the volume of patients that in the future will travel by ambulance to CRH. The impact of additional ambulance capacity required will be taken into account by commissioners during future contracting discussions with the Yorkshire Ambulance Service.
6.5 Workforce Assumptions
As previously described the Trust faces considerable workforce challenges which undermine the resilience of clinical services, staff satisfaction and wellbeing, and the Trust’s finances. This SOC has assumed that the reconfiguration of clinical services across the two hospital sites will enable the Trust to:
- Reduce duplicate staffing costs through the consolidation of some services;
- Improve clinical rota resilience and reduce the frequency of on-call;
- Allow greater opportunities for sub-specialisation of the workforce;
- Improve the recruitment and retention of clinical staff;
- Reduce reliance on Agency staffing;
- Enable development of new roles and improved workforce skill mix;
- Enable optimised use of digital technology to support delivery of care;
- Improve workforce productivity including theatre utilisation;
- Improve junior doctor and other staff training experience and supervision.
As a result of the above the reconfiguration of services will deliver a more efficient and effective use of workforce resource.
6.6 Travel Assumptions
In May 2017 a Travel and Transport Group was established with an independent Chairperson and wide ranging membership to consider and develop plans to address the implications of any proposed changes in the configuration of hospital services in relation to public access, travel, parking and transport.
This SOC aims wherever possible to maintain services on both hospital sites to provide the best access for local people, unless this means that we cannot provide the best quality of care. A final report was published by Travel and Transport Group in January 2018. The report escribed the changes in travel times likely to be experienced (by car, taxi and public transport) to CRH and HRI as shown below.
Private Transport comparative Journey Times (80% of patients or visitors travel to hospital by car or taxi)
| Travel by car/taxi from: | Maximum average journey times in minutes | |||
|---|---|---|---|---|
| Based on actual data | Based on modelled data assuming people travel to a different location | |||
| Calderdale postcodes | To CRH | 17.6 minutes | To HRI | 24 minutes |
| Kirklees postcodes | To HRI | 15.1 minutes | To CRH | 20.5 minutes |
Public Transport comparative Journey Times (20% of patients or visitors travel to hospital by public transport)
| Travel by public transport from: | Maximum average journey times in minutes | |||
|---|---|---|---|---|
| Based on actual data | Based on modelled data assuming people travel to a different location | |||
| Calderdale postcodes | To CRH | 52.7 minutes | To HRI | 66.1 minutes |
| Kirklees postcodes | To HRI | 46.3 minutes | To CRH | 65.8 minutes |
The review also noted that the average journey time along the A629 section between the two hospitals is approximately 13 minutes and that journey times should improve following the upgrade of the A629 (currently in progress) and reduce travel times by 4 to 4.5 minutes.
The Travel and Transport Group noted that an Equality Impact Assessment had determined there was no indication of differential impact that would lead to unlawful discrimination and concluded that work on changes in the configuration of hospital services should continue to be progressed.
The Travel and Transport Group recommended a number of actions to be taken in relation to parking, access, travel between hospitals, public transport, reducing need to travel, hospital discharge, patient travel and greener transport. The list of recommendations is shown below.
Report of the Independent Chair of the Travel and Transport Group – 30 January 2018
Recommendations
- That the strategic direction set in Right Care, Right Time, Right Place, continues to be implemented with an emphasis on shifting the focus of health and social care services closer to home reducing reliance on Acute Health Service setting at local Hospitals.
- Regular updates of the progress being made on implementation of Care Closer to Home, the A629 upgrade and a local Travel and Transport Plan should be highlighted in the local NHS Communication Strategy.
- That the Calderdale and Greater Huddersfield CCGs continue to work through their existing engagement channels in line with each CCGs’ ‘Engagement and Experience Strategy for local people’ to seek advice and feedback on Travel and Transport issues to influence the implementation of the report’s recommendations.
- The upgrade of the road network and the proposed reconfiguration of health services are challenging and complex parallel projects which require active management throughout the 5 year transition period. We recommend the local NHS consider identifying a Board Level Transport Champion to work in partnership with Calderdale and Kirklees Councils, WYCA and other key players to develop a coherent travel plan which sets out strategy, measures, action plans and targets to maximise alignment of both projects and to develop a sustainable and integrated Transport Strategy.
- The West Yorkshire Combined Authority should bring to the attention of Commercial Bus Companies the opportunities created by the Road Transport Upgrade and the proposed reconfiguration of health services to secure more direct and frequent services between the hospitals and local transport hubs promoting a more integrated transport system.
- The action plan outlined for short term and longer term action to address parking issues should be implemented and the feasibility of additional multi-storey car parking at CRH evaluated.
- We recommend that the Shuttlebus service is upgraded with:
- a) Immediate action on advertising the service, signage and timetables, adequate weatherproof shelters and enhanced patient and public experience.
- b) A more equitable service is developed meeting the needs of vulnerable people, people with disability and wheelchair users as well as infants, children and their parents / carers.
- c) Consideration of a more frequent service with greater capacity and exploration of links between both Hospitals and local transport hubs to contribute to a more integrated transport system.
- 8. Improvements to the Patient Transport Service outlined in the Future Action section are implemented in a timely way consistent with Patient and Public feedback.
Greater Huddersfield CCG and Calderdale CCG are currently leading work with partners to address and implement actions in response to these recommendations. This includes establishing a steering group to oversee the work. The Trust will be a member of this Group and support necessary actions in response to the recommendations.
7. Estate Options And Assumptions
The Trust is a community and hospital multi-site organisation. It provides services from a number of buildings across Calderdale and Greater Huddersfield. Acute hospital services are provided from two sites which are approximately 5 miles apart: Huddersfield Royal Infirmary (HRI) in Huddersfield and Calderdale Royal Hospital (CRH) in Halifax.
Pennine Property Partnership (a property joint venture of the Trust with Henry Boot Developments) undertook the development of Acre Mill (which is located across the road from HRI). Acre Mill was opened as an outpatient centre in 2015. Both hospital sites contain clinical and non-clinical accommodation which varies considerably in terms of type, age and quality.
7.1 Calderdale Royal Hospital – Overview of Current Estate
Calderdale Royal Hospital (CRH) has a gross floor area of 59,817m2 across a site with land area of 7.36 acres. CRH is located close to Halifax town centre and opened in 2001. The hospital offers a full range of outpatient facilities as well as inpatient areas including Surgical, Medical, Maternity, ICU, Coronary Care and Children’s wards. CRH currently has circa 450 beds and 9 theatres including 8 main theatres and an emergency Obstetrics theatre. The Dales Unit on the CRH site is occupied by South West Yorkshire Partnership Foundation Trust and includes three in-patient wards as well as a number of outpatient services. The site was one of the first hospitals built through PrivateFinance Initiatives (PFI).
Work commenced in January 1999 and the building was handed over to the Trust in March 2001. Parts of the old Halifax General Hospital buildings were retained and refurbished and in general these are used for office accommodation. The hospital was built by the Catalyst Healthcare consortium, which then comprised the Lend Lease Corporation, Bovis Lend Lease Limited, ISS Mediclean Limited, the British Linen Bank Limited and the French bank Societe Generale. Bovis Lend Lease provided the design and construction services.
As part of the PFI agreements are in place with Engie for estates maintenance, life cycle and variation work and with ISS for the provision of catering, cleaning, portering, security, car park management, switchboard and linen distribution. The Trust works closely with all parties to ensure close and open partnership working. In 2005 the car parking facility was extended to include the South Car Park and barrier car parking was introduced to try to assist with access to the hospital for patients and visitors. In 2010 a new Endoscopy Unit was completed and two years later saw the development of a new angio suite incorporating state of the art catheter lab at Calderdale. In 2013 the installation of a new CT Scanner took place and a year later a new coronary care advanced pacing theatre opened. In 2015 the child development unit was completely refurbished to allow the merger of the services from Huddersfield and Calderdale. Through the Engie life cycle programme new chiller units were installed in the roof plant area in 2009 bringing improved efficiency and noise management by modern pump technology and controls. In the last 5 years, Theatre operating lights; Passenger Lift cars; CCTV; Security Access systems; Fire detection; Doors & Windows have all received replacement and upgrade through Planned Life Cycle investment. The whole site is subject to planned replacement of flooring; fitted furniture and redecoration. In January 2016 Engie began a medical gas plant replacement programme which has seen the upgrade of 4bar medical air, 7bar surgical air and vacuum plant bringing new equipment and increased resilience to the site. This work also coincided with the upgrade and replacement of critical ventilation systems incorporating requirements of the most recent healthcare technical guidance.
The revenue costs of the site include interest and hard and soft facilities management. The total annual revenue cost is circa £23m. The backlog maintenance is managed through the PFI contract and supported by regular capital lifecycle payments into the PFI provider. Building maintenance is managed through the SPC and funded through regular planned lifecycle payments. There is limited backlog maintenance of note and the building is compliant to NHS Estates Code condition B.
7.2 Huddersfield Royal Infirmary – Overview of Current Estate
Huddersfield Royal Infirmary (HRI) has a gross floor area of 67,493m2 across a site with land area of 16.77 acres. Huddersfield Royal Infirmary is about two miles from Huddersfield town centre. The main hospital opened in 1965 and since then many millions have been invested in the site to modernise and extend it.
The hospital offers a full range of day case and outpatient services; an accident and emergency department, and critical care. It is currently the centre for emergency surgery, planned complex surgery and emergency paediatric surgery for the people of Greater Huddersfield and Calderdale (these services are not currently provided at CRH). It also provides a full range of diagnostic services including magnetic resonance imaging (MRI). There are approximately 420 beds at HRI.
Recent major developments have included the opening of a £3.4 million urology unit and investment in a £500,000 state-of-the-art CT (computerised tomography) scanner and suite. Early in 2008 the new Huddersfield Family Birth Centre opened at the hospital, offering a warm and friendly environment for women and their partners. In 2008 an £8 million pharmacy manufacturing unit opened on the site which produces pharmaceutical products for people across the country and is expected to continue to provide services in the future. A new state of the art endoscopy unit was built in 2011 and the Trust embarked on a scheme to replace the ageing calorifiers with plate heat exchangers which was completed in 2015. In 2016 a full upgrade of services for oncology outpatients and day-case patients in the newly named Greenlea Ward was completed.
A full refurbishment of inpatient theatres was completed in 2017, bringing the main theatres into a fully compliant state. The Trust owns the Acre Mill site opposite Huddersfield Royal Infirmary and this new development for out patients’ services was opened in 2015.
The Trust has upgraded many of the inpatient wards, giving additional single rooms with ensuite facilities. Although there has been significant investment, the core building is considered to be beyond its useful life and is time expired. Financial pressures have placed significant restraints on capital investment in recent years and, as a result, the backlog of maintenance for time expired buildings requirement has grown.
Backlog maintenance, with regards to the HRI site, refers to the costs associated with time expired buildings. The cost described in this section is the minimum investment required to bring the estate to a category B level. In 2013 the Trust commissioned a 6 facet survey from NIFES Consulting Group; this was updated by Lendlease Consulting in 2015. It identified the extent of capital works required to bring HRI to condition B status in accordance with the Department of Health Estate code. The survey concluded that the Estate is overall in poor condition with significant backlog of maintenance for time expired buildings. The survey identified statutory items across the site that required immediate remedial action in large parts of the estate as well as key factor impacting on operational performance. A significant investment is required to resolve the functional suitability of the estate. This has been driven through changes in service provision and size of teams that has meant the parts of the current estate are too small or were constructed and designed for another function which does not provide a suitable layout and space for services.
The Trust carries a very high risk in terms of the condition and reliability of buildings at HRI. Some are not clinically fit for purpose and without capital injection there is a very high risk of failure of critical estate services and consequent impact on service delivery. The 2015 updated survey estimated the costs to bring the estate to a level B at £95m. Since 2015 there has been a further deterioration of the estates building and engineering service infrastructure and space/functional suitability. An updated 6 facet survey has been commissioned and the report from this will be available in 2019 and will inform the development of the Outline Business Case.
7.3 Estate options considered to deliver the Hospital Service Model
The proposed future model of hospital services described in this SOC will make use of both existing hospitals as follows:
- Both hospitals will provide 24/7 A&E services and a range of day-case, outpatient and diagnostic services.
- One hospital will receive all blue light emergency ambulances for patients that have serious life-threatening conditions and all patients likely to require acute non-elective hospital admission.
- One hospital will provide elective services and surgery as well as providing step-down medical inpatient beds.
Consideration of which hospital site should focus on unplanned inpatient care and which site on planned care has been debated for a number of years. In 2015 the Trust, supported by Monitor and Ernst Young, developed the Trust’s Five Year Strategic Plan. This work included an appraisal of eleven possible estate options for the future development of a planned and unplanned hospital site. The clinical service model is not site dependent and, therefore, an appraisal of whether unplanned inpatient care would be provided at the CRH or HRI site was required.
On the basis of the qualitative and financial appraisal undertaken, the choice of CRH as the unplanned site and HRI as the planned site was approved by the Trust Board in 2015 and was the single estate option on which public consultation was undertaken in 2016.
The service model on which the estate option appraisal was previously undertaken in 2015 has been modified in this SOC to take account of the views and concerns of stakeholders and the IRP. However, the question of which site should be developed to provide unplanned acute inpatient services and which to provide planned inpatient care services remains the same. This SOC has therefore used the significant work previously undertaken to assess estate options and is based on CRH being expanded to provide unplanned inpatient care and HRI providing planned inpatient care services.
7.4 The Estate Cost Model
A total capital investment requirement of £196.5m has been identified that is based on:
- £20m at HRI to enable adaptation of existing buildings and to address immediately the most critical maintenance requirements to enable the continued use of some of the HRI existing site thereby deferring new build at this site for at least 10 years. The detailed use of this investment will be informed by the updated 6 Facet Survey that is currently being undertaken. Key areas of investment are likely to include the upgrade of A&E resuscitation, ward areas, windows, stone cladding, air handling, pipe work, fire safety, drains and asbestos removal.
- £176.5m for expansion and new build at CRH – this estate cost is based on work undertaken in May 2017 by Lendlease Consulting that provided the Trust with a Feasibility Cost Model of the expected build costs for the future development of the CRH site. The cost estimates were based on the gross internal floor areas derived from a schedule of accommodation prepared by a Healthcare Planner in discussion with the Trust on the required clinical activity and capacity.
The cost of the future model at CRH and at HRI is shown in the table below. This is based on estate feasibility costing previously undertaken by Lendlease in 2017. This has been reviewed (with advice provided by NHS England Project Appraisal Unit) to update the assumptions used for inflation in building costs and fees and the level of optimism bias that has been applied.
| Element | CRH Cost (£) | HRI Cost (£) | Total Cost (£) |
|---|---|---|---|
| CRH | £74,695,800 | £74,695,800 | |
| Site infrastructure | £2,975,360 | £2,975,360 | |
| Traffic management | £115,948 | £115,948 | |
| External works | £700,120 | £700,120 | |
| Service diversions | £140,000 | £140,000 | |
| Access and logistics | £173,922 | £173,922 | |
| Links | £1,575,000 | £1,575,000 | |
| Sustainability | £686,756 | £686,756 | |
| Section 106/278 | £772,988 | £772,988 | |
| Sub-total | £81,835,894 | £81,835,894 | |
| Preliminaries | £12,661,445 | £12,661,445 | |
| Fees | £13,912,102 | £13,912,102 | |
| Non works costs | £1,546,505 | £1,546,505 | |
| Equipment costs | £5,155,017 | £5,155,017 | |
| Planning contingency | £16,612,686 | £16,612,686 | |
| Optimism bias (%) | £26,344,730 | £26,344,730 | |
| Sub-total | £158,068,379 | £158,068,379 | |
| Inflation | £18,478,194 | £18,478,194 | |
| VAT | £35,309,315 | £35,309,315 | |
| VAT recovery | -£35,309,315 | -£35,309,315 | |
| Total | £176,546,573 | £176,546,573 | |
| Backlog maintenance | - | £20,000,000 | £20,000,000 |
| Total (including backlog) | £176,546,573 | £20,000,000 | £196,546,573 |
| Disposals | - | - | 0 |
| Total capital requirement | £176,546,573 | £20,000,000 | £196,546,573 |
The estate cost model provides for:
- Beds: A total capacity of circa 840 beds (broadly the same as current) across the two sites. The number of beds open at any point in time will fluctuate dependent on demand through the year. Within this total are included 18 ICU beds with the ability to increase this to 22 in future years.
- Theatres: A total of 19 theatres (11 at CRH and 8 at HRI). This will provide an additional emergency obstetric theatre at CRH which was recommended by the CQC. As explained in section 3.4 no provision has been included for the development of a hybrid vascular theatre.
Based on advice provided by NHS Improvement additional car parking at CRH will be developed through alternate sources of capital funding via a partnership with either a public or commercial joint venture. CRH currently has 787 car parking spaces. The proposed development will provide an additional 600 space multi-storey car park at CRH, and establish an additional 80 spaces at Dryclough Close (both subject to planning permissions). This would give a total of 1467 spaces. It is estimated that the development of the CRH site would result in a loss of 134 spaces. The net total parking spaces would therefore be 1,333 representing a growth of 546 compared to current (787).
7.5 Feasibility of the New Build Development at CRH
During February and March 2019 the Trust has undertaken work to confirm feasibility of the scale of the estate new build development required at the CRH site. This work has been informed by professional external engineering and architecture advice and has confirmed the previous work undertaken in 2017 that the proposed scale of expansion at CRH can be accommodated on the site.
The illustration below of the CRH site indicates in green where the new build expansion will be located. The learning and development centre shown in red will be re-provided within the new build accommodation. Additional multi-storey car parking will be provided at the front of the hospital.
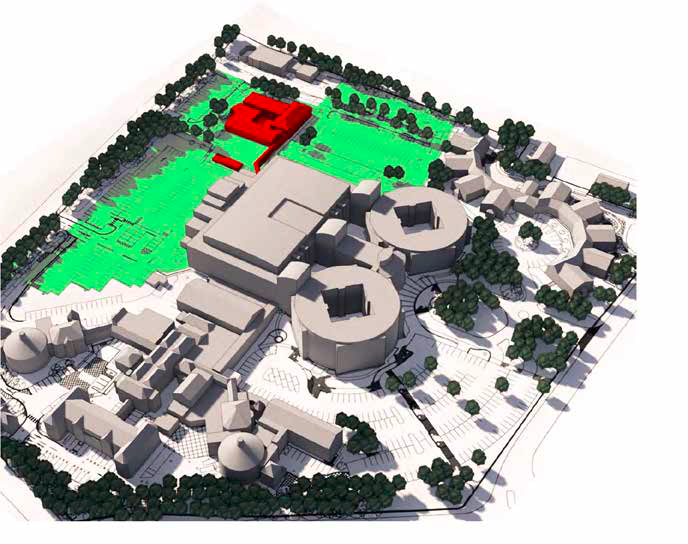
The estate developments proposed will be designed to enable the optimal use of new technology and digital communications to enable ‘real-time’ review and advice on patient’s care to be provided by specialist staff at either hospital site and in the community.
This will amplify the benefits of service reconfiguration and support achievement of the Trust’s aim to make the best use of technology to support care closer to home, complemented by a hospital model that provides essential clinical adjacencies and the critical mass required to sustain staff recruitment, ensure quality and develop revenue savings.
8. Economic Case
8.1 Summary
The purpose of the economic case is to identify and economically appraise the options for the delivery of the proposed service and estate model that is most likely to offer best value for money.
8.1.1 Approach to evaluation
The option appraisal described in this SOC builds on significant work jointly undertaken in a number of meetings and workshops held in 2015 by the Trust and the two Clinical Commissioning Groups (CCGs) (supported by Monitor, NHS England and Ernst Young) to identify and appraise a long list of possible estate options for the future development of a planned and unplanned hospital site – rejecting options that would not be financially, operationally or clinically viable.
The appraisal included qualitative analysis (involving commissioners and stakeholders) against the following benefits criteria:
- Clinical benefits;
- Patient pathways;
- Patient travel times;
- Capital requirements;
- Bed capacity;
- Wider health economy forecasts;
- Commissioning intentions.
The appraisal was also informed by Monitor’s advice that options requiring either DH and Treasury support to buy-out the existing PFI agreement, or that would result in an under-utilisation of the high cost PFI facilities at CRH, would not be supported on the grounds of being un-economic.
8.2 The Option analysis framework
The table below describes the criteria used to appraise the long list of options.
| Critical Success Factors | Description |
|---|---|
| Scope of Service | Able to deliver the full scope of the proposed service configuration i.e.:
|
| Service solution | Makes best use of the existing estate at both hospital sites and improves the environment of care for patients. |
| Service Delivery | Enables the continued delivery by the Trust of core DGH services for the local population. |
| Service implementation | Enables the delivery of the defined scope of services in the shortest possible timescale recognising the urgency of the need for change (as referenced by the IRP). |
| Funding Availability | Able to be delivered within the available funding source and envelope |
8.3 Estate Long List Evaluation
The following long list of twelve estate options has been considered and options discounted as shown if they do not meet the essential criteria.
| Option | Configuration | Scope | Service Solution | Service Delivery | Service Implementation | Funding | Conclusion |
|---|---|---|---|---|---|---|---|
| 1 | Business As Usual Minimum change in hospital configuration across two sites but incorporates known changes that will occur in next 5 years (e.g. demographic, tariff impacts, initiatives unrelated to hospital reconfiguration), with the Trust operating its capital programme within its own generated sources e.g. prior loan level and Joint Venture investment. | No | No | Yes | No | Yes | Carry forward |
| 2 | Do Minimum | No | No | Yes | No | No | Carry forward |
| 3 | All Hospital Services at CRH All existing hospital services provided at CRH i.e. a single hospital site proposal. Dispose of HRI and Acre Mill sites. | No | No | No | No | No | Discount |
| 4 | All Hospital Services at CRH enabled by a reduced range of services provided by CHFT The Trust reduces activity to ensure all services can be delivered from CRH site only i.e. single hospital site proposal. Dispose of HRI and Acre Mill sites. | No | No | No | No | No | Discount |
| 5 | All Hospital Services at HRI – Use Break Clause to exit PFI All hospital services provided at HRI i.e. a single hospital site proposal. Exit CRH site through use of PFI break clause at 2031. | No | No | No | No | No | Discount |
| 6 | All Hospital Services at HRI. Trust sublets / finds alternate use of CRH to secure income to cover PFI cost. All hospital services provided at HRI i.e. a single hospital site proposal. Alternate use of CRH secured. | No | No | No | No | No | Discount |
| 7 | Intermediate Option – A&E and unplanned care at CRH. A&E and Planned care at HRI on main site. £177m development at CRH and a £20m investment in HRI, reflecting the reduced usage of the site. A&E at both sites. | Yes | Yes | Yes | Yes | Yes | Carry forward |
| 8 | Emergency and unplanned care at CRH. Planned care at Huddersfield on Acre Mill site. CRH provides all emergency, unplanned and high risk care. Planned services are provided in Huddersfield on Acre Mill site (dispose of main site). No A&E Department at HRI. | No | No | No | No | No | Discount |
| 9 | Emergency and unplanned care at HRI. Planned care at CRH. | No | No | No | No | No | Discount |
| 10 | Emergency and unplanned care at HRI. Planned care at CRH with any under-utilised PFI estate sublet. HRI provides all acute and emergency care and high risk care. Planned care services are provided at CRH site and alternate use is found for some of the CRH estate to optimise PFI utilisation and improve affordability. No A&E Department at CRH. | No | No | No | No | No | Discount |
| 11 | Do Maximum - All Hospital Services in a New build Exit CRH, HRI and Acre Mill sites and build new hospital at new site delivering all services. | No | No | No | No | No | Discount |
| 12 | Growth of activity and income on both sites to improve financial & clinical viability negating the need to reconfigure services. Maximise income from both sites via increased activity and market share to enable improved income and financial viability. | No | No | Yes | No | No | Discount |
8.3.1 Economic Case Long List Conclusion
The Long List analysis above outlines the options that are available to the Trust to meet the service and estate requirements. In further evaluating the options available to the Trust the intention is to evaluate a short list option of:
- Base Case;
- Do Minimum; and
- Intermediate Option (Future Service Model Option) - Emergency and unplanned care at CRH. A&E and Planned care at HRI on main site.
The following sections refer to these options as Option A - Base Case; Option B - Do Minimum and Option C - Future Service Model.
8.4. Appraisal / Evaluation Methodology
Continuing with the existing service model under a Business As Usual or Do Minimum option is non-viable in the long-term as it does not meet any of the core requirements of the Trust, nor is the finance available to support the required capital investment to sustain safe services. Business As Usual and Do Minimum serve however as a baseline to assess the benefit of the evaluated option and demonstrate that the Future Model Option is the most economically advantageous option.
Each of the evaluated options has been based on:
- The base year and price year is FY20;
- Prices exclude VAT;
- Cash flows and benefits are discounted by 3.5% per annum to reflect social time preference; and
- Although, build/refurbishment timelines are different a 65 year appraisal period has been used, which reflects the re-development period plus 60 years of operation.
8.4.1 Cost
There are a number of steps involved in arriving at a proposed economic option. Traditional discounted cash flows across the following categories are considered for each option:
- Capital Outlays: for new builds or refurbishment are applied by year of spend.
- An estimate of the residual value of an asset - at the end of the lifespan to represent an estimate of an asset’s value at that time, i.e. 60 years.
- Capital and revenue lifecycle costs - of maintaining estate assets.
- The Trust’s capital programme - for new and replacement assets.
- Revenue cost cash flows - across clinical, non-clinical and estates costs across the lifetime.
- Transitional costs - declared separately and consider non-recurrent or ad-hoc spends.
- Externalities – costs have been reflected within the evaluation for the impact of the case on other external parties.
The sum of these discounted results creates an Equivalent Annual Cost (EAC) by option. A ranking occurs with the lowest EAC receiving the Agreed option status.
8.4.2 Revenue Costs
Revenue costs have been driven from the 2019/20 operational plan submitted to NHSI in February 2019 for the base year and reflect activity changes for future modelled years. All other options have been considered to assess the degree to which they might be different to the baseline position. Typical areas considered include:
- Transition costs for reconfiguration – non-recurring, project and dual running forecasts have been modelled. These costs are estimated at £10m;
- Project management costs across the Trust;
- Dual running staffing costs, backfill and training costs; and
- Revenue lifecycle estimates over a 65 year period.
8.4.3 Capital costs
Capital cash-flow is specific to each option and includes:
- Estimates for new capital build;
- Major refurbishment estimates;
- Capital lifecycle trajectories;
- Internal replacement capital programme forecasts;
- Internal new and replacement equipment requirements.
8.4.4 Residual Value Calculations
An estimate of the value of new build assets has been included to discount costs 65 years. Residual values for estate have been assumed to be equivalent to the value of land for each site. This assumption is consistent within all options
8.4.5 Externalities
The impact on other organisations has been considered and modelled within the economic assessment.
The economic case excludes the impact on commissioners of QIPP delivery as the cost of enabling QIPP delivery is unknown at this point. This is excluded in all options and therefore does not become a differentiator within the economic assessment. Equally if QIPP delivery costs become known it is anticipated that they would be allocated by the same amount across each option.
8.5 Net Present Cost and Equivalent Annual Cost Analysis
The table below provides a summary of the Net Present Cost (NPC) for each of the options under evaluation, assessed over 65 years.
| £m | Business As Usual | Do Minimum | Future Service |
|---|---|---|---|
| Option A | Option B | Option C | |
| £m | £m | £m | |
| Net Present Cost (NPC) | (£10,256.86) | (£10,213.19) | (£10,449.52) |
| Rank | 2 | 1 | 3 |
8.5.1 Net Present Cost conclusion
The conclusion from the Net Present Cost assessment is that the Do Minimum Option has the lowest Net Present Cost. This conclusion is drawn when assessed at 65 years. The evaluation of risks and benefits are assessed below.
8.6. Benefits overview
8.6.1. Approach
The identified benefits are based on key benefits deliverable across the period of the business case and have been developed with the Economic Adviser from the Department of Health. The benefits identified are classified between cash releasing benefits and societal benefits and include:
- Pay savings, efficiency and productivity;
- New roles and models of care;
- Reduction in estate costs;
- Reduction in length of stay through efficiency;
- Reduced patient transport between sites;
- Societal benefits delivered through reduced length of stay.
The identified benefits will be further developed, with additional benefits identified as the Trust completes the procurement, financing, management case, risk management and benefits realisation as the Trust moves to the next steps to develop the business case.
| £m | Business As Usual | Do Minimum | Future Service |
|---|---|---|---|
| Option A | Option B | Option C | |
| NPC | NPC | NPC | |
| Sunk costs | - | £1.6 | |
| Appraisal– Cash releasing benefits | - | £93.58 | £241.1 |
| Sub-total and variance to Business As Usual | - | £93.58 | £242.7 |
| Societal benefits | - | £7.76 | |
| Total benefits and Variance to Business As Usual | - | £93.58 | £250.46 |
| Variance to Do Minimum | (93.58) | 156.88 | |
| Rank | 3 | 2 | 1 |
8.6.1.1 Do Minimum Benefits
Within the Do Minimum case additional cash releasing benefits are required to be delivered to ensure the Trust remains in financial balance, to off-set the cost of the spend on backlog maintenance. The ability of the Trust to realise these savings is considered within the risk section below.
8.6.1.2 Future Service Model Benefits
Within the Future Service Model is a financial benefit associated with the design costs for the redevelopment. These are sunk costs that are a benefit in continuing with the Future Service Model option. Identified cash releasing benefits enabled through the reconfiguration of services are quantified benefits. These benefits are:
- Skills mix and reduction in agency premium;
- Improved operational efficiency including staffing rotas;
- Reduced estate costs and transport costs.
Identified societal benefits from reconfiguration are:
- Job creation in the local area;
- Improvement in lives and well-being;
- Improved patient care outcomes;
- Reduced patient and staff transfers.
Each of the benefits above have been quantified and included within the economic evaluation.
8.6.2 Benefits Review Conclusion
The identified benefits outline a favourable cash releasing and societal benefits delivered through the Future Service Model option when compared to both the Business As Usual and Do Minimum options.
8.7. Risk overview
8.7.1. Approach
An exercise has been undertaken to assess identified risks associated with the reconfiguration of services across the Calderdale Royal Hospital and Huddersfield Royal Infirmary. The Trust quantified the risk by assessing the weighting, probability and risk retention/transfer of the following risk categories:
- Design Risks;
- Construction and Development Risks;
- Performance Risks;
- Operating Cost Risks;
- Variability of Revenue Risks;
- Termination Risks;
- Technology and Obsolescence Risks;
- Control risks;
- Residual Value Risks;
- Other Project Risks;
- Additional Project Risks.
The output of this assessment has informed the Net Present Cost (NPC) for each evaluated option.
8.7.2 Risk Assessment
| £m | Business As Usual | Do Minimum | Future Service Model |
|---|---|---|---|
| Option A | Option B | Option C | |
| NPC | NPC | NPC | |
| Design Risks | £0.00 | £0.00 | (£7.33) |
| Construction and Development Risks | £0.00 | £0.00 | (£18.88) |
| Performance Risks | £0.00 | £0.00 | (£12.79) |
| Operating Cost Risks | £0.00 | £0.00 | (£9.59) |
| Variability of Revenue Risks | (£118.59) | (£118.59) | (£118.59) |
| Termination Risks | £0.00 | £0.00 | £0.00 |
| Technology and Obsolescence Risks | (£69.09) | (£69.09) | (£69.09) |
| Control risks | £0.00 | £0.00 | £0.00 |
| Residual Value Risks | £0.00 | £0.00 | £0.00 |
| Other Risks | £0.00 | £0.00 | (£0.03) |
| Additional Project Risks | (£628.26) | (£555.90) | (£268.04) |
| Risk adjusted NPC | (£815.94) | (£743.59) | (£504.36) |
8.7.3 Quantified Risk Overview
The key variation to the Business As Usual and Do Minimum options are the risks associated with the capital investment i.e. the design, construction, performance and operating cost risk associated with a new build. These have been quantified and are adverse risks within the Future Service Model.
Additional project risks include:
- Requirement for Emergency Capital expenditure;
- Inability deliver additional CIP savings without reconfiguration;
- Requirement for a new build development at HRI;
- Operational service impact of building failure at HRI.
Of the additional project risks greater quantified risk exists within the Business As Usual and Do Minimum options as the Trust reflects the risk of not investing within the aging HRI estate. Whilst the quantified risk is lower in the Do Minimum case, reflecting the investment within the existing site, this remains higher than the Future Service Model due to the reconfiguration of services and the focused investment in the HRI site.
8.7.4 Risks Review Conclusion
The risk assessment identifies that the Future Service Model is a lower cost risk model and is favourable when compared to the Business As Usual and the Do Minimum options.
8.8. Conclusions from the Economic Case
| - | Business As Usual | Do Minimum | Future Service Model |
|---|---|---|---|
| Option A | Option B | Option C | |
| £m | £m | £m | |
| Net Present Cost (NPC) | (£10,256.86) | (£10,213.19) | (£10,449.52) |
| Rank | 2 | 1 | 3 |
| Benefits Adjustment (NPC) | £93.58 | £250.46 | |
| Benefits Adjusted Net Present Cost (NPC) | (£10,256.86) | (£10,119.61) | (£10,199.06) |
| Benefits Adjusted Rank | 3 | 1 | 2 |
| NPC Risk Adjustment | (£815.94) | (£743.59) | (£504.36) |
| Risk and Benefits Adjusted Net Present Cost (NPC) | (£11,072.80) | (£10,863.20) | (£10,703.42) |
| Benefits and Risk Adjusted Rank | 3 | 2 | 1 |
It is concluded that Option C (Future Service Model) is the Agreed option. The Economic Case analysis reaffirms the case for change set out within the Case for Change, i.e. that the development of CRH as the unplanned hospital, with a planned hospital and emergency care centre development at HRI provides economic, value for money (VFM) advantage compared to the Business As Usual and Do Minimum options. Further evaluation of risks and benefits will be carried out as the reconfiguration business case develops.
9. Commercial Case
The Commercial Case described in this chapter provides a high level approach to the procurement of the capital development works. This will be developed in more detail in the Outline Business Case.
The DHSC has announced 100% public capital funding is available and this is the preferred funding route for the development. The choice of a procurement route must meet the Trust’s needs, project requirements and ensure the optimal management of risk for the Trust.
The Trust also wishes to ensure that the procurement strategy and contract(s) support the development of collaborative relationships between the Trust and its suppliers. The Trust has considered the elements of capital works required for the proposed development. This requirement can be described as:
- Reconfiguration of the existing CRH PFI site; infrastructure works required to the existing CRH building to integrate the existing site into the new build, including the expansion of hospital areas e.g. Emergency Department.
- New build works at CRH outside the scope of the PFI project; to increase the estate footprint to accommodate the increase in unplanned care on the CRH site.
- Capital investment at HRI; to enable adaptation of existing buildings and to address immediately the most critical maintenance requirements to enable the continued use of some of the existing site.
There are two important issues the Trust has considered in determining the preferred procurement route and subsequent contract management for the delivery of these capital estate developments:
- The role of Calderdale and Huddersfield Solutions Ltd (CHS);
- The Trust’s current legal and contractual arrangements for the existing PFI at Calderdale Royal Hospital.
9.1 The Potential Role of CHS Ltd in the Procurement and Contract Management
Calderdale and Huddersfield Solutions Ltd (CHS) was incorporated as a registered company limited by shares on 15th March 2018. The sole shareholder is CHFT and CHS is therefore a wholly owned subsidiary of the Trust. CHS provides a fully managed suite of healthcare facilities for use by CHFT and provides value to CHFT through its specific service offering and through its ability to manage developments and operational risk for the Trust and other parties. CHS is led by a directly employed Managing Director and employs approximately 450 staff providing specialist estates, facilities, procurement and contract management services on behalf of CHFT and other customers. CHS’s status as a “Teckal” trading company means that the Trust is able to contract directly with CHS without the need for a competitive procurement process.
The Trust’s preferred approach at this stage is to instruct CHS to act on behalf of the Trust to deliver the necessary procurement(s) and subsequent contract management of suppliers to deliver the estate capital development works described above.
This approach will be further defined in the Outline Business Case and will include consideration of the procurement options available to the Trust to ensure it secures best value in the future provision of services.
9.2 The Trust’s Current Legal and Contractual Arrangements for the Existing PFI
The Trust has sought to understand the options available for the procurement of the capital works to ensure that they are feasible in relation to the existing PFI contractual and legal arrangements and the Trust has concluded that:
- The reconfiguration of the existing CRH facilities will be procured by way of a variation of the existing PFI Project;
- The Trust has flexibility to deliver its proposals in respect of the new build works at CRH and the work at HRI under a single procurement process which would: avoid duplicating procurement costs; improve the likelihood of delivering both developments in accordance with a timetable determined by the Trust; and create a single counterparty for the Trust to deal with. However, it is possible for them to be procured separately and to follow different models. The procurement approach will therefore allow for flexibility and provide the opportunity for suppliers to bid for CRH; HRI; or CRH & HRI.
9.3 Statutory and Regulatory Procurement Compliance
The Trust will as necessary secure specialist advice to ensure the Trust takes full account of, changes in procurement legislation and processes post Brexit.
9.4 Market Soundings
The ability of the Trust to secure value for money through procurement will be influenced by the ability to attract sufficient credible bidders to generate and maintain meaningful competition throughout the procurement process. Accordingly, the Project will be carefully marketed to attract potential bidders. This will include pre-market engagement to enable discussion about scope and commercial issues; to ensure that the project is attractive to bidders; to explain proposed design methodology, including timescales so that bidders can resource it; and discuss proposed bid deliverables and evaluation criteria at each stage.
9.5 Trust Capability and Approach
The Trust has previous experience of delivering major procurement projects on a competitive dialogue basis. This includes for example:
- Procurement of the Cerner Electronic Patient Record, across two Trusts working with Bradford Teaching Hospitals NHS Foundation Trust;
- Establishing the Pennine Property Partnership (a property joint venture of the Trust with Henry Boot Developments) to undertake the development of Acre Mill (which is located across the road from HRI). Acre Mill was opened as an outpatient centre in 2015.
Trust Board members and other senior leaders in the Trust have a breadth of relevant experience that will support and enable delivery of the project.
This includes, for example, experience of leading and delivering the following major projects:
- Broad Street Complex (Halifax);
- Shay Stadium (Halifax);
- Piece Hall (Halifax);
- Brighouse & Sowerby Bridge Leisure facilities;
- Large Scale Voluntary Transfer (LSVT) of Housing (Rossendale);
- Independent Sector Treatment Centre for North Bradford PCT;
- Community hospitals for North Bradford PCT;
- Integration of the three NHS Leeds CCGs to create one Commissioning organization;
- Acre Mills Outpatient development - Pennine Property Partnership;
- Establishing Calderdale and Huddersfield Solutions Ltd (CHS) – a wholly owned subsidiary of CHFT;
- North of England Housing Market Renewal Regeneration;
- Major development and refurbishment programmes for a National Housing Association;
- Development of Calderdale Royal Hospital through a PFI initiative;
- Transforming Community Services - Calderdale Community Services;
- Hospital redevelopment at Nuffield Cambridge, Bristol, Newcastle-upon-Tyne, Chester;
- High Bay Warehouse at Trentham Gardens Stoke-on-Trent;
- Factory extension at Scunthorpe;
- Tesco new store development;
- Hospice at Peterborough;
- Global £500m transformation programme for a major insurance company;
- Procurement and management of multiple large outsourcing contracts in the private and public sector;
- Major IT programmes in support of major changes in public services;
- ‘Building Better Health for Bolton’ NHS LIFT Programme;
- Leading the establishment and development of the Commission for Health Improvement;
- Metrolink expansion programme;
- International relocation of a professional services (dot com) company;
- Previous significant experience of service reconfiguration including major trauma services in West Yorkshire.
Project management and governance arrangements will be established. The Trust will seek legal and specialist advice as necessary to plan and navigate through the Procurement approach.
10. Financial Case
10.1 Introduction
The purpose of the financial case is to set out the indicative financial implications of the Agreed option as concluded within the Economic Case. The financial case is underpinned by the Trust’s FY20 operational concluded within the Economic Case. The financial case is underpinned by the Trust’s FY20 operational plan as submitted to NHSI in February 2019.
The preparation of the ‘Agreed Service Option’ modelled within the financial case have been modelled based on the NHS Operational Planning and Contracting Guidance 2019-20 with assumptions made to evaluate the financial case over a 25 year period.
The Trust recognises its current deficit financial position and that the Business As Usual and Do Minimum modelled options leave the Trust with an unsustainable clinical model and an unsustainable level of estate risk.
The financial models and assumptions used within the financial case are derived from the Trust’s activity trajectories which are integrated within the Trust’s operational plans.
The Agreed Service Option demonstrates a return on investment and enables the Trust to return to a cash generating financial position, an improved longer term financially sustainable position that addresses the key service and estate risks.
The Financial Case is based on Option C (Future Service Model) however it includes Option A (Business As Usual) and Option B (Do Minimum) for comparative purposes.
10.2 Impact on the Trust’s Income and Expenditure Account
The summary financial impact of the Agreed Service Option is outlined in the table below:
| - | FY27 | FY45 |
|---|---|---|
| Agreed Service | Agreed Service | |
| Option C | Option C | |
| £m | £m | |
| Total Revenue | 437.0 | 576.9 |
| Total Operating Expenditure | (396.3) | (529.2) |
| EBITDA | 40.7 | 47.7 |
| Total Non-operating Expenses | (36.5) | (28.9) |
| Net Surplus / (Deficit) | 4.2 | 18.8 |
| Net Surplus / (Deficit) margin (%) | 1% | 3% |
10.3 FY19 Financial Performance – Forecast to 31 March 2019
The Trust continues to forecast delivery of the planned deficit of £43.1m. The key risks associated with delivery of the FY19 plan are:
- The high risk associated with CIP schemes to the value of £0.24m;
- The costs associated with additional winter pressures have been included within the plan and forecast, but there remains a small risk that these exceed the available budget.
10.4 Financial Assumptions Overview
10.4.1 Key Assumptions Underpinning the Financial Case
The Financial Case modelled is based on the Trust’s FY20 Operational Plan submitted to NHSI in February 2019. The other key assumptions within the Financial Case are detailed below.
10.4.2 Key Income & Expenditure (I&E) Assumptions
The key assumptions within the forecast are:
- That the Trust will receive £7.33m Provider Sustainability Fund (PSF) allocation. This is assumed in FY20 only in line with current Trust plans;
- That the Trust will receive £14.807m Financial Recovery Fund (FRF) allocation. This is assumed in FY20 in line with current Trust plans and it is assumed that a further £7.33m (previously received as PSF) is received from FY21 in future years to the value the Trust is in deficit, but not greater than £22.137m in total;
- The Trust will receive Marginal Rate Emergency Tariff (MRET) at £6.147m in 2019/20 only. This funding, at the same value is assumed to have transferred within PbR tariff from 2020/21 onwards;
- The Trust will deliver CIP efficiency savings of between 1.1% and 3.0% per annum throughout the financial case, with £10m net reconfiguration savings delivered post reconfiguration;
- Transitional costs of £10m will be incurred over the period of reconfiguration.
10.4.3 Key Growth Assumptions
Growth assumptions have been modelled within the financial plan for future years based on a review of three year historic growth trends and commissioner intentions over future years. The following growth assumptions are assumed for future years:
- Day case – 0%
- Elective – 0%
- Outpatient activity – 0%
- Emergency Department – 2%
- Non-elective short-stay admissions – 4%
- Non-elective long-stay admissions – 1%
- Community – 2%
These growth assumptions drive the income assumptions for the Trust from Greater Huddersfield CCG and Calderdale CCG. This is shown in the next section.
10.4.4 Commissioner Affordability
The Trust has shared the activity, growth and inflation assumptions of the SOC with its two key commissioners for transparency and to ensure overall affordability of the SOC for the West Yorkshire healthcare sector. The following table sets out the clinical income values per commissioner over the five year period.
| £m | FY20 | Y21* | FY22 | FY23 | FY24 | FY25 |
|---|---|---|---|---|---|---|
| Year | Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 |
| CHFT Calderdale CCG Income | 145.4 | 151.5 | 154.9 | 158.5 | 162.1 | 165.8 |
| CHFT Greater Huddersfield CCG Income | 130.2 | 135.7 | 138.6 | 141.7 | 144.9 | 148.1 |
| CHFT Clinical Income | 275.6 | 287.2 | 293.5 | 300.2 | 307.0 | 313.9 |
| Calderdale CCG | 145.4 | 151.5 | 154.9 | 158.5 | 162.1 | 165.8 |
| Greater Huddersfield CCG | 130.2 | 135.7 | 138.6 | 141.7 | 144.9 | 148.1 |
| CHFT Clinical Income | 275.6 | 287.2 | 293.5 | 300.2 | 307.0 | 313.9 |
| Greater Huddersfield CCG variance | - | - | - | - | - | - |
| Calderdale CCG variance | - | - | - | - | - | - |
| Difference | - | - | - | - | - | - |
For FY19 and FY20 the Trust and Commissioners agreed an Aligned Incentive Contract for the year. The contract recognises the unsustainable financial position of the West Yorkshire health economy and overall financial constraints of the NHS. The key principles of the contract are to reduce the overall cost of healthcare to the health economy through collaborative working and innovation.
The Trust is committed to delivering a financially sustainable solution for the health sector in West Yorkshire. Through the Partnership Transformation Board the Trust is working with commissioners to identify and deliver QIPP that delivers financial savings for the health system i.e. both the commissioners’, and providers’, expenditure is reduced through the delivery of the QIPP, supporting the AIC contractual relationship
10.4.5 Financial Assumptions
The projections laid out in the Financial Case include a number of assumptions around how the Trust operates:
- Pay/Non-pay split – where costs have not been able to be directly attributed to pay and non-pay categories, these have been split on a proportionate basis to pay/non-pay expenditure.
- Marginal cost – the assumption has been that any growth or movement in activity will have a marginal cost impact of 70%.
- Working – none of the options is assumed to have any significant impact on the Trust’s working capital policy (i.e. payables and receivables days remain constant throughout the Plan period).
10.4.6 Economic Assumptions
The Trust has also made a number of economic assumptions governing cost inflation and tariff deflation. These are presented below.
| - | FY21-FY45 |
|---|---|
| Year | Yr 1 |
| Clinical Income | 1.51% |
| Other Income | 1.0% |
| Pay & Incremental drift | 3.1% |
| Drugs | 0.6% |
| CNST | 1.0% |
| Clinical Supplies & Other non-pay | 1.8% |
These assumptions are based on the recurrent inflationary factors within the FY20 national PbR tariff. Any changes that may arise on these assumptions in the future will not materially impact the
financial option appraisal since changes to such assumptions will impact the Existing Service model and Agreed Service Option materially equally.
10.4.7 Capital Assumptions
Estimates for capital expenditure were obtained from the work undertaken by Lendlease Consulting for the costs associated with CRH. Capital expenditure estimates are based on the gross internal floor areas of the development, taken from the Schedule of Accommodation produced by the Healthcare Planner following confirmation of the proposed service changes under the Proposed Option. HRI capital
10.4.7.1 Impairment of Capital Expenditure
A 15% impairment of the expenditure on new works at CRH (i.e. capital expenditure excluding backlog maintenance) is assumed on completion of the works (in FY25). HRI is assumed to be impaired by 50% in value post reconfiguration, reflecting the reduced utilisation of the estate (in FY26).
10.4.7.2 Depreciation policy for capital expenditure
- Reconfiguration capital – depreciated over 40 years;
- Backlog maintenance capital – depreciated over 34 years (current average for HRI).
10.4.7.3 Asset Disposals
There are no asset disposals planned beyond those planned in FY20.
10.4.7.4 Capital Estimate Inclusions
All of the below are pro-rated across the breakdown of capital provided by the Quantity Surveyor:
- Preliminary costs – 15%;
- Professional fees – 17%;
- Non-works costs – 1.9%;
- Capital equipment costs – 6.3%;
- Planning contingency – 20.3%;
- Optimism bias – 20%;
- Inflation – 11.7%;
- Value Added Tax (VAT) – 20%.
10.4.7.5 Revaluations
Revaluations have been assumed to occur to the Trust’s estate. The estate is first revalued in FY21, and then annually thereafter to maintain the estimated market value of the estate.
10.4.8 Cash Assumptions
Throughout each of the modelled options the Trust is reliant on additional Revenue Support Loans in the period prior to returning to financial surplus. This has been modelled with an interest charge of 1.5%, which is the current rate of the borrowing for the Trust for this facility. As existing loans are repaid these are assumed as replaced at new loans at 1.5%. The Trust’s Revenue Support Loan is assumed to be repayable over 35 years, based on cash availability to the Trust to make loan repayments.
10.4.9 Financing Assumptions
10.4.9.1 Option A – Business As Usual
Investment to address HRI back-log maintenance is delivered within the internally generated capital resource from FY21 onwards. FY20 includes emergency capital funding at £2.4m in line with the Trust’s FY20 Operational Plan.
10.4.9.2 Option B – Do Minimum
- Back-log maintenance investment addresses the High and Significant at a cost of £60m over 10 years, funded through Emergency Capital loans.
- Emergency Capital loans are funded at 1.94% over 10 years.
10.4.9.3 Option C – Agreed Option
- £196.6m development funded through PDC.
- Interim capital loans utilised prior to the approval of the FBC, which are repaid once PDC is received.
10.5 Summary Financial Expenditure
The summary financial impact of the Agreed Service Option (Option C) is outlined in the table below:
| £m | FY27 | FY45 |
|---|---|---|
| Agreed Service | Agreed Service | |
| Option C | Option C | |
| £m | £m | |
| Total Revenue | 437.0 | 576.9 |
| Total Operating Expenditure | (396.3) | (529.2) |
| EBITDA | 40.7 | 47.7 |
| Total Non-operating Expenses | (36.5) | (28.9) |
| Net Surplus / (Deficit) | 4.2 | 18.8 |
| Net Surplus / (Deficit) margin (%) | 1% | 3% |
The total capital expenditure on the reconfiguration of services is £196.6m of capital expenditure.
10.6 Capital Costs
The table below is the capital expenditure plans submitted to NHS Improvement, with the addition of the expenditure planned on the Option C strategic reconfiguration. Detailed capital planning has been performed by the Trust for FY20 and outline plans identified for FY21-FY25.
| £m | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | |
| HRI Estates and backlog maintenance | 2.4 | 5.0 | 4.0 | 3.6 | 3.0 | 2.0 | ||||||
| CRH Strategic Reconfiguration | 1.6 | 3.0 | 2.0 | 44.9 | 82.6 | 42.5 | ||||||
| NPEx* | 1.3 | |||||||||||
| NHS Energy Efficiency Fund (NEEF)* | 0.7 | |||||||||||
| PFI – Lifecycle | 1.7 | 1.8 | 0.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Capital Programme** | 13.7 | 7.6 | 7.6 | 8.3 | 8.2 | 8.1 | 11.1 | 10.8 | 10.3 | 9.9 | 9.4 | 15.3 |
| Donated Assets | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 1.3 |
| Total | 21.6 | 17.6 | 14.0 | 56.9 | 94.0 | 52.8 | 11.3 | 11.0 | 10.5 | 10.1 | 9.6 | 16.6 |
10.6.1 Detailed Capital Plan – Agreed Service Model Option C
The table below provides a detailed analysis of the costs associated with the Agreed Service option.
| Element | CRH Cost (£) | HRI Cost (£) | Total Cost (£) |
|---|---|---|---|
| CRH | £74,695,800 | £74,695,800 | |
| Site infrastructure | £2,975,360 | £2,975,360 | |
| Traffic management | £115,948 | £115,948 | |
| External works | £700,120 | £700,120 | |
| Service diversions | £140,000 | £140,000 | |
| Access and logistics | £173,922 | £173,922 | |
| Links | £1,575,000 | £1,575,000 | |
| Sustainability | £686,756 | £686,756 | |
| Section 106/278 | £772,988 | £772,988 | |
| Sub-total | £81,835,894 | £81,835,894 | |
| Preliminaries | £12,661,445 | £12,661,445 | |
| Fees | £13,912,102 | £13,912,102 | |
| Non works costs | £1,546,505 | £1,546,505 | |
| Equipment costs | £5,155,017 | £5,155,017 | |
| Planning contingency | £16,612,686 | £16,612,686 | |
| Optimism bias (13%) | £26,344,730 | £26,344,730 | |
| Sub-total | £158,068,379 | £158,068,379 | |
| Inflation | £18,478,194 | £18,478,194 | |
| VAT | £35,309,315 | £35,309,315 | |
| VAT recovery | (£35,309,315) | (£35,309,315) | |
| Total | £176,546,573 | £176,546,573 | |
| Backlog maintenance | - | £20,000,000 | £20,000,000 |
| Total (including backlog) | £176,546,573 | £20,000,000 | £196,546,573 |
| Disposals | - | - | 0 |
| Total capital requirement | £176,546,573 | £20,000,000 | £196,546,573 |
Backlog maintenance at HRI will seek to address the very high risk areas of the estate that require action in the short to medium term. The expenditure will be focused on resuscitation intensive care unit, four ward areas and external building works. The Trust will utilise its available capital resource in future years to maintain the site beyond the short/medium term.
10.6.2 Impairment
| £m | FY25 | FY26 |
|---|---|---|
| CRH Unplanned site | (26.5) | - |
| HRI site | - | (36.8) |
| Revaluation reserve | - | 20.5 |
| Impairment Charge to I&E | (26.5) | (16.3) |
The capital investment in new buildings typically costs more than the value of the building. The assumption used within the financial model is a reduction in asset value of 15%. In addition an impairment of the existing HRI site, recognising the reduced utilisation of the HRI footprint has been assumed to be 50% of the value. This is consistent with the Trust’s experience of impairments on significant new build costs.
The impairment charge arising from reconfiguration has been treated as an exceptional item within the financial model.
10.7 Detailed Financial Expenditure – Affordability (Option C – Agreed Option)
The activity, workforce and capital plans are modelled within the financial expenditure table below:
10.7.1 Income and Expenditure Account
| - | - | Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical Revenue | 319.3 | 332.7 | 345.4 | 352.2 | 359.3 | 366.6 | 374.1 | 380.2 | 386.3 | 392.7 | 398.8 | 405.1 | 514.0 |
| Non Protected/Non Mandatory Clinical Revenue | 7.3 | 6.2 | 6.3 | 6.5 | 6.6 | 6.8 | 6.9 | 7.1 | 7.3 | 7.4 | 7.6 | 7.8 | 11.0 |
| Other Revenue | 39.0 | 40.5 | 40.9 | 41.3 | 41.7 | 42.1 | 42.5 | 43.0 | 43.4 | 43.8 | 44.3 | 44.7 | 51.9 |
| PSF / FRF | 28.3 | 22.1 | 19.2 | 12.1 | 7.0 | 9.4 | 2.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Total Revenue | 365.6 | 407.6 | 414.7 | 419.2 | 419.8 | 422.6 | 433.0 | 432.4 | 437.0 | 443.9 | 450.7 | 457.6 | 576.9 |
| Employee Benefit Expenses | (253.3) | (259.5) | (260.4) | (261.8) | (262.4) | (264.1) | (272.5) | (268.6) | (269.2) | (271.4) | (276.9) | (282.6) | (383.1) |
| Drugs | (37.2) | (38.1) | (37.5) | (37.0) | (36.4) | (35.8) | (35.3) | (35.0) | (34.6) | (34.5) | (34.3) | (34.2) | (32.2) |
| Clinical Supplies & Services | (30.0) | (29.5) | (29.4) | (29.4) | (29.3) | (29.2) | (29.2) | (29.3) | (29.3) | (29.5) | (29.8) | (30.0) | (33.8) |
| Other Expenses | (51.2) | (50.5) | (49.8) | (49.1) | (49.1) | (47.3) | (47.2) | (47.1) | (47.0) | (47.1) | (47.4) | (47.8) | (80.2) |
| PFI Operating Expenses | (12.8) | (13.3) | (13.6) | (13.7) | (14.1) | (14.6) | (15.0) | (15.5) | (16.1) | (16.3) | (16.7) | (17.3) | (0.0) |
| Total Operating Expenditure | (384.4) | (391.0) | (390.8) | (391.0) | (391.2) | (391.1) | (399.3) | (395.5) | (396.2) | (398.7) | (405.2) | (411.8) | (529.2) |
| EBITDA | (18.8) | 16.6 | 23.9 | 28.2 | 28.5 | 31.5 | 33.7 | 36.9 | 40.7 | 45.2 | 45.5 | 45.8 | 47.7 |
| EBITDA Margin (%) | (5.1%) | 4.1% | 5.8% | 6.7% | 6.8% | 7.5% | 7.8% | 8.5% | 9.3% | 10.2% | 10.1% | 10.0% | 8.3% |
| Gain/(loss) on asset disposals | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Impairment Losses (Reversals) net | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | (26.5) | (16.3) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Depreciation & Amortisation | (11.7) | (11.5) | (11.6) | (11.8) | (12.0) | (12.1) | (12.1) | (15.3) | (15.3) | (15.3) | (15.3) | (15.3) | (15.3) |
| Interest / Contingent Rent | (10.4) | (11.6) | (12.2) | (12.9) | (13.3) | (13.7) | (14.0) | (14.2) | (14.5) | (14.8) | (15.0) | (15.2) | (0.0) |
| Intreset payable on Loans | (2.4) | (3.2) | (3.4) | (3.2) | (2.7) | (2.5) | (2.4) | (2.3) | (2.2) | (2.1) | (2.0) | (1.9) | (1.0) |
| PDC Dividend | 0.0 | (0.0) | (0.0) | (0.0) | (0.3) | (3.0) | (5.0) | (4.8) | (4.3) | (4.7) | (5.1) | (5.6) | (12.4) |
| Other Non-Operating | 0.3 | 0.0 | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) |
| Total Non-operating | (24.2) | (26.3) | (27.4) | (28.1) | (28.4) | (31.4) | (60.0) | (53.2) | (36.5) | (37.1) | (37.7) | (38.2) | (28.9) |
| Net Surplus / (Deficit) | (43.0) | (9.6) | (3.5) | 0.1 | 0.1 | 0.1 | (26.4) | (16.3) | 4.2 | 8.1 | 7.8 | 7.6 | 18.8 |
| Net Surplus / (Deficit) margin (%) | (12%) | (2%) | (1%) | 0% | 0% | 0% | (6%) | (4%) | 1% | 2% | 2% | 2% | 3% |
| Normalised (excluding impairments / Disposals) | (43.0) | (9.6) | (3.5) | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 4.1 | 8.1 | 7.8 | 7.6 | 18.8 |
10.7.1.1 Option C – Agreed Service Model Financial overview
Financial modelling of the Agreed Service model option shows the Trust return to financial surplus in FY22 however the Trust remains reliant on Financial Recovery Fund (FRF) until FY26. The Trust returns to a financial surplus on a recurrent basis in FY27 as the benefits of reconfiguration are realised and the Trust delivers CIP recurrently.
Revenue increases year on year by the growth in activity assumed along with the clinical income tariff increases. This is somewhat offset by efficiency improvements in length of stay to maintain activity within the Trust’s existing bed base from FY26. The Trust’s expenditure decreases in real terms in FY26-FY28 through realisation of reconfiguration benefits and CIP across the period, including delivery of skills mix to ensure the Trust has a workforce to meet the clinical requirements. Other changes in the income and cost base are driven by the economic assumptions.
Impairments arise in the financial plan in FY25 and FY26 as a consequence of estate reconfiguration. Impairment arises from impairing the existing HRI site and new capital build on completion.
10.7.2 Cost Improvement Programme (CIP)
The Trust has strong governance processes for the planning, monitoring and delivery of CIP and a track record of achievement. This was confirmed by NHSI following their CIP ‘deep-dive’ visit to the Trust in June 2017 and Use of Resources assessment in March 2018.
The Trust allocates CIP targets to operational and corporate divisions using a range of national and local benchmarking data in a deliberate approach to ensure allocation of CIP targets is based on evidence of where there may be efficiency opportunity (as opposed to simply a prorata share of target to budgets). ‘Portfolio’ opportunities (cross cutting or transformational
schemes that impact on more than one operational division or require external partnerships) are led by a Director who is accountable for delivery.
Based on the targets allocated individual CIP schemes are progressed through detailed planning stages with weekly formal review of progress undertaken by the Trust’s Turnaround Executive and monthly review at the Trust’s Finance and Performance Committee.
In the three years FY17 to FY19 annual CIP delivery has ranged between £15m and £18m per annum resulting in a total of £50.9m efficiency savings realised across the three year period. The FY20 CIP plan assumes the Trust delivers £11m in CIP and revenue generation schemes. It is in the context of successful historic delivery of CIP; long term strategic change enabled by the reconfiguration plans; and the future opportunities afforded the organisation by working collaboratively across the region that the Trust will strive to achieve the financial plan for FY20.
The FY20 CIP plan assumes delivery of £11.0m CIP and internal, as well as West Yorkshire wide, planning will support this.
The CIP programme for FY20 has now been identified in full.
10.7.2.1 Reconfiguration Benefits
Reconfiguration allows the delivery of services in a more sustainable way and supports the deployment of both reduced and alternative workforce models. Overall the proposed reconfiguration releases a further £10m of costs over and above existing CIP plans. The majority of the costs relate to clinical workforce costs. The clinical model proposed does increase the establishment required for the delivery of Emergency Departments to support improved clinical rotas and increased consultant presence. This is achieved through skill mix of the entire workforce and use of new roles. Consultant establishment will be increased in line with Royal College Guidance to support both the increased un-planned activity on the CRH site but also the remaining activity on the HRI site. This will lead to more favorable rotas, recruitment and ultimately less reliance on agency and high cost temporary staffing.
Elsewhere within medical specialties, the proposed model centralises services and removes the need for a number of sub-specialty out of hours rotas. This again supports recruitment and reduction in overall agency and temporary staffing costs. Other material benefits arise from the investment in modern ward and bed stock. Ward sizes are planned at optimal efficiency bed numbers rather than existing 1960s configured wards which do not support efficient nurse to bed ratios.
The creation of one single critical care unit will deliver efficiencies through skill mix and the move to a planned activity site at HRI releases theatre costs both out of hours but also in supporting improved productivity. This improved productivity will create capacity to repatriate work from private sector and can then be absorbed within existing theatre capacity.
Whilst overall clinical rotas for anesthetists remain the same as present, increasing rotas at CRH and reduced rotas at HRI allows for deployment of new clinical roles at CRH such as Physicians Associates. This is a further efficiency that is not deliverable in the current configuration. As for medical specialties, the development of a planned site at HRI enables centralisation of a number of sub specialty surgical rotas on the unplanned care site at CRH.
The Trusts continued investment in digital technology enables further efficiency within support services within the proposed new clinical model. Out of hours support at HRI is reduced and the site is supported either remotely or through use of point of care testing and automatic release of blood through Blood Track. The investment into the new clinical model will ensure a modernised approach to delivery of outpatient activity. Digital technology will be used to reduce the need to attend hospital and further enhance the Trusts ambition to improve outpatient flow and experience. This releases additional costs and drives further outpatient efficiency.
Investment into the HRI site will be made to both make the site safe but also to reduce the operational footprint at HRI and disengage elements of the site that are both beyond useful life and economic repair. This will allow reduced costs both in terms of maintenance, upkeep and capital charges.
10.7.2.2 Other Initiatives
From FY21 the local system will have embedded new ways of working in Greater Huddersfield and Calderdale across community and hospital services. This collaboration will enable efficiencies to be achieved in relation to administration, management, and property costs.
10.7.3 Cost Improvement Programme (CIP)
The table below outlines the required CIP across the period FY20 – FY45.
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Actual | Plan | Plan | Plan | Plan | Plan | Plan | Plan | Plan | Plan | Plan | Plan | Plan | |
| CIP | 18.0 | 11.0 | 9.0 | 9.0 | 9.0 | 9.0 | 9.0 | 5.7 | 5.6 | 3.9 | 3.9 | 4.0 | 5.4 |
| Reconfiguration benefits | 2.0 | 4.0 | 4.0 | ||||||||||
| WYAAT | 2.1 | 2.0 | 3.1 | 2.1 | |||||||||
| TOTAL – Planned efficiencies | 18.0 | 11.0 | 11.1 | 11.0 | 12.1 | 11.1 | 9.0 | 7.7 | 9.6 | 7.9 | 3.9 | 4.0 | 5.4 |
| Planned cumulative efficiencies | 18 | 29.0 | 40.1 | 51.1 | 63.2 | 74.4 | 83.4 | 91.1 | 100.7 | 108.6 | 112.5 | 116.4 | 185.6 |
| Efficiency % of Operating Expenditure | 4.7% | 2.8% | 2.8% | 2.8% | 3.1% | 2.8% | 2.3% | 1.9% | 2.4% | 2% | 1% | 1% | 1% |
10.7.4 Use of Resources (UoR) metrics – Single Oversight Framework NHS Improvement
NHSI has now introduced the Single Oversight Framework (SOF). Where previously a separate Finance rating (the FSRR) and Governance rating were issued, these are brought together under the SOF. This considers 5 themes: Quality of Care; Finance and use of resources; Operational performance; Strategic change; Leadership and improvement capability. The Finance element of this system is the Use of Resources score and the constituent parts of this measure are described below.
- Liquidity: days of operating costs held in cash or cash-equivalent forms (cash in the bank less payables plus receivables, on the presumption these can be immediately converted into cash);
- Capital servicing capacity: the degree to which the organisation’s generated income covers its financing obligations a measure of the Trust’s ability to afford its debt - in this sense payments against debts include PDC payments, interest and loan repayments and PFI interest, PFI contingent rent and PFI capital repayments;
- Income and expenditure (I&E) margin: the degree to which the organisation is operating at a surplus/deficit (measured against the Control Total which excludes impairments, gains/losses on disposal and donated assets);
- Variance from plan in relation to I&E margin: variance between a foundation Trust’s planned I&E margin in its annual forward plan and its actual I&E margin within the year (again measured against the Control Total which excludes impairments, gains/losses on disposal and donated assets);
- Agency: measurement of actual agency usage against the original agency ceiling set by NHSI at the planning stage. A distance from target of greater than 50% results in the lowest rating of 4 against this metric.
| - | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liquidity | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 3 | 1 |
| Capital servicing capacity | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 3 | 3 | 3 | 3 | 1 |
| I&E Margin | 4 | 4 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| I&E Margin variance | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Agency | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Overall UoR score | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 |
10.7.5 Statement of Financial Position over 25 years (FY20 – FY45)
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Property, Plant and Equipment | 227.8 | 236.4 | 243.9 | 249.5 | 297.5 | 382.7 | 400.3 | 363.0 | 362.6 | 362.2 | 361.8 | 361.3 | 360.9 |
| Inventories | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 | 7.1 |
| NHS Trade Receivables | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 | 8.4 |
| Non NHS Trade Receivables | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 | 9.5 |
| Other Current Assets | 6.1 | 13.8 | 13.8 | 12.8 | 10.3 | 8.5 | 9.3 | 6.8 | 6.1 | 6.1 | 6.1 | 6.1 | 6.1 |
| Cash and Cash Equivalents | 1.9 | 1.9 | 2.0 | 2.0 | 3.0 | 2.9 | 2.8 | 2.7 | 6.6 | 10.7 | 14.5 | 18.1 | 21.5 |
| Current assets | 32.9 | 40.7 | 40.7 | 39.7 | 38.2 | 36.4 | 37.1 | 34.4 | 37.6 | 41.7 | 45.5 | 49.1 | 52.5 |
| Total assets | 260.7 | 277.0 | 284.7 | 289.2 | 335.8 | 419.0 | 437.4 | 397.5 | 400.2 | 403.9 | 407.3 | 410.4 | 413.4 |
| Current Liabilities | (43.5) | (44.0) | (45.5) | (45.5) | (45.4) | (45.6) | (45.7) | (45.9) | (46.3) | (46.6) | (47.0) | (47.4) | (46.9) |
| Non-Current Liabilities | (217.9) | (240.3) | (248.5) | (249.5) | (226.6) | (220.8) | (217.5) | (210.6) | (204.9) | (195.7) | (186.1) | (175.9) | (168.9) |
| Total Liabilities | (261.5) | (284.3) | (293.9) | (295.0) | (272.0) | (266.4) | (263.2) | (256.4) | (251.2) | (242.3) | (233.1) | (223.3) | (215.8) |
| Net assets employed | (0.8) | (7.3) | (9.2) | (5.8) | 63.8 | 152.7 | 174.2 | 141.0 | 149.1 | 161.5 | 174.2 | 187.1 | 197.6 |
| Public dividend capital | 117.0 | 120.1 | 120.1 | 120.1 | 186.5 | 272.1 | 316.6 | 316.6 | 316.6 | 316.6 | 316.6 | 316.6 | 316.6 |
| Retained Earnings (Accumulated Losses) | (156.6) | (166.2) | (169.7) | (169.6) | (169.5) | (169.4) | (195.8) | (212.1) | (207.9) | (199.8) | (192.0) | (184.4) | (176.9) |
| Revaluation reserve | 38.8 | 38.8 | 40.3 | 43.7 | 46.8 | 50.0 | 53.4 | 36.5 | 40.3 | 44.7 | 49.5 | 54.8 | 57.9 |
| Total taxpayers’ equity | (0.8) | (7.3) | (9.2) | (5.8) | 63.8 | 152.7 | 174.2 | 141.0 | 149.1 | 161.5 | 174.2 | 187.1 | 197.6 |
10.7.6 Cash Flow Statement
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Cash flows from operating activities | (19.0) | 16.2 | 23.5 | 27.8 | 28.1 | 31.1 | 33.2 | 36.9 | 40.3 | 44.8 | 45.1 | 45.4 | 47.2 |
| Cash generated from (used in) operations | 2.5 | (10.0) | 0.2 | 1.2 | 2.5 | 1.8 | (0.8) | 2.4 | 0.9 | 0.0 | 0.0 | 0.0 | 0.0 |
| Cash generated from (used in) investing activities | (10.5) | (17.6) | (17.4) | (13.8) | (56.7) | (93.8) | (52.5) | (11.0) | (10.8) | (10.3) | (9.8) | (9.4) | (15.3) |
| Cash generated from (used in) financing activities | 26.9 | 11.3 | (6.3) | (15.2) | 27.1 | 60.8 | 20.0 | (28.3) | (27.2) | (31.1) | (32.1) | (33.1) | (17.6) |
| Increase/ (decrease) in cash and cash equivalents | (0.1) | 0.0 | 0.1 | 0.0 | 1.0 | (0.1) | (0.1) | (0.0) | 3.3 | 3.4 | 3.1 | 2.9 | 14.4 |
10.7.7 Sensitivity Analysis
The Trust has considered variants to the business case as sensitivities based on the potential opportunities and risks that may arise within the local health economy. The following table highlights the bottom line deficit projections for the Agreed Service option. In the table below, the following non recurrent items have then been stripped out of these deficits to show the underlying (recurrent) deficit positions in each year:
- Net I&E Impairments of £26.5m in FY25 and £16.3m in FY26; and
- Non-recurrent costs of £10m;
| Deficit £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Agreed option (deficit)/surplus | (43.0) | (9.6) | (3.5) | 0.1 | 0.1 | 0.1 | (26.4) | (16.3) | 4.2 | 8.1 | 7.8 | 7.6 | 18.8 |
| Impairments (I&E impact) | 26.5 | 16.3 | |||||||||||
| Non-recurrent costs | 0.3 | 1.5 | 1.1 | 6.9 | 0.2 | ||||||||
| Normalised (deficit)/surplus | (43.0) | (9.6) | (3.5) | 0.4 | 1.6 | 1.2 | 7.0 | 0.2 | 4.2 | 8.1 | 7.8 | 7.6 | 18.8 |
10.7.7.1 Downside Sensitivities
The following downside scenarios have been considered by the Trust:
- Downside 1 – Financial Recovery Fund (FRF) reduction
FRF income is non-recurrent revenue that is only confirmed in FY20 however the Trust has assumed receipt of £72.0m across FY21-FY26. If the Trust was limited to 50% of the assumed FRF across the same period the Trust would remain in deficit until FY24, returning to surplus in FY25 for one year, report a deficit in FY26 and then deliver recurrent surpluses from FY27 onwards. - Downside 2 – Increase in Dual Running Costs
The Trust has assumed non-recurrent transition costs of £10m associated with the reconfiguration. These are assumed as pay costs, consistent with the 5 Year Strategic Plan to support transitional project management. These costs are based on an initial assessment however this estimate could increase over and above, for the sensitivity this has been assumed to increase to £15.1m. - Downside 3 – Increase in cost basis arising due to external factors
The Trust has modelled inflationary factors within the financial case as outlined in section 12.5.6. Due to current political uncertainty surrounding the UK and its relationship with the EU post BREXIT, there remains a risk that a rise in costs could occur above the assumed inflationary factors, or fall in the value of the pound, which is not funded through national tariff. Each 1% increase in nonpay costs would create a £1.3m cost pressure to the Trust from FY20. This cost pressure has been assumed to exist for three years, a cumulative impact of £3.9m. - Downside 4 – Marginal Rate Emergency Tariff decrease
The Trust is assuming that MRET will transfer into PbR tariff from FY21 onwards in full at £6.147m. A risk exists that this value does not transfer in full, potentially up to £2m per annum. - Downside 5 – Non-delivery of WYAAT CIP initiatives
The Trust through collaboration with WYAAT has identified a number of CIP initiatives that could deliver financial efficiencies for the Trust totaling £9.2m. WYAAT are committed to working collaborative to operate efficiencies non-delivery of these schemes are potential downside to the Trust’s financial position.
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normalised (deficit)/surplus | (43.0) | (9.6) | (3.5) | 0.4 | 1.6 | 1.2 | 7.0 | 0.2 | 4.2 | 8.1 | 7.8 | 7.6 | 18.8 |
| Reduction in FRF income by 50% | (11.1) | (9.6) | (6.1) | (3.5) | (4.7) | (1.1) | |||||||
| Increase in dual running site costs | (1.0) | (2.0) | (2.0) | ||||||||||
| Increase in cost basis arising due to external factors | (1.3) | (2.6) | (3.9) | (3.9) | (3.9) | (3.9) | (3.9) | (3.9) | (3.9) | (3.9) | (3.9) | ||
| MRET decrease | (2.0) | (2.0) | (2.0) | (2.0) | (2.0) | (2.0) | (2.0) | (2.0) | |||||
| Non-delivery of WYAAT CIP initiatives | (2.1) | (2.0) | (3.1) | (2.1) | |||||||||
| Sub - total movement | (14.5) | (14.2) | (13.1) | (12.5) | (12.6) | (9.0) | (5.9) | (5.9) | (5.9) | (5.9) | (5.9) | ||
| Downside case surplus/(deficit) | (43.0) | (9.6) | (18.0) | (13.8) | (11.5) | (11.3) | (5.6) | (8.8) | (1.7) | 2.2 | 1.9 | 1.7 | 12.9 |
10.7.7.2 Upside Sensitivities
The following upside scenarios have been considered by the Trust:
- Upside 1 Increased CIP
The Trust has forecast increased CIP delivery in FY26-FY28 post reconfiguration. A potential upside is that the Trust can increase CIP delivery post reconfiguration rather than the three years currently modelled. This would deliver £3.4m in FY28 and an additional £3.4m in FY29, a total cumulative benefit of £6.8m. - Upside 2 – Realisation of LoS, QIPP and Community benefits
The Trust has an opportunity to improve its length of stay (LoS) from the current performance to the upper quartile, realised through the benefits of reconfiguring services across its Halifax and Huddersfield sites. The benefits of this are an £8m improvement to the Calderdale and Huddersfield health economy. The Trust has assumed that £5m of this benefit remains with the Trust to contribute to the Trust’s overall deficit position. This has been assumed to be realised from FY25. - Upside 3 – Aligned Incentive Delivery
The Trust has an aligned incentive contract with its two key commissioners. The contract seeks to maximise the efficiency of delivery of healthcare for our local population with benefits of the contract shared between the Trust and the CCG’s. Through working together, further cost reduction for the healthcare system could exceed current plans, with a further benefit to the Trust. A potential upside could be a share benefit of 1% of the contract value per annum.
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normalised (deficit)/surplus | (43.0) | (9.6) | (3.5) | 0.4 | 1.6 | 1.2 | 7.0 | 0.2 | 4.2 | 8.1 | 7.8 | 7.6 | 18.8 |
| Increased CIP delivery post reconfiguration | 3.4 | 6.8 | 6.8 | ||||||||||
| Improvement in LoS following reconfiguration | 1.0 | 3.0 | 5.0 | 5.0 | 5.0 | 5.0 | |||||||
| Aligned Incentive contract benefit | 2.9 | 2.9 | 3.0 | 3.1 | 3.1 | 3.2 | 3.2 | 3.3 | 3.3 | 3.4 | 3.4 | ||
| Sub - total movement | 2.9 | 2.9 | 3.0 | 3.1 | 3.1 | 4.2 | 6.2 | 8.3 | 11.7 | 15.2 | 15.2 | ||
| Upside case surplus/(deficit) | (43.0) | (9.6) | (0.6) | 3.3 | 4.6 | 4.3 | 10.1 | 4.4 | 10.4 | 16.4 | 19.5 | 22.8 | 34.0 |
10.8 Detailed Financial Expenditure – Affordability (Option A – Business as Usual)
For comparison, the activity, workforce and capital plans for the Business As Usual Option are modelled within the financial expenditure table below:
10.8.1 Income and Expenditure Account
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Clinical Revenue | 319.3 | 332.7 | 345.4 | 352.2 | 359.3 | 366.6 | 374.3 | 380.0 | 385.8 | 391.8 | 397.9 | 404.2 | 512.5 |
| Non Protected/Non Mandatory Clinical Revenue | 7.3 | 6.2 | 6.3 | 6.5 | 6.6 | 6.8 | 6.9 | 7.1 | 7.3 | 7.4 | 7.6 | 7.8 | 11.0 |
| Other Revenue | 39.0 | 40.5 | 40.9 | 41.3 | 41.7 | 42.1 | 42.5 | 43.0 | 43.4 | 43.8 | 44.3 | 44.7 | 51.9 |
| PSF / FRF | 28.3 | 22.1 | 18.4 | 9.8 | 2.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Total Revenue | 365.6 | 407.6 | 414.7 | 418.4 | 417.4 | 417.9 | 423.8 | 430.1 | 436.5 | 443.1 | 449.8 | 456.7 | 575.4 |
| Employee Benefit Expenses | (253.3) | (259.5) | (260.4) | (261.5) | (261.9) | (263.0) | (267.9) | (272.0) | (276.1) | (281.5) | (286.9) | (292.5) | (390.8) |
| Drugs | (37.2) | (38.1) | (37.5) | (37.0) | (36.4) | (35.8) | (35.6) | (35.3) | (34.9) | (34.8) | (34.6) | (34.4) | (31.9) |
| Clinical Supplies & Services | (30.0) | (29.5) | (29.4) | (29.4) | (29.3) | (29.2) | (29.4) | (29.5) | (29.6) | (29.8) | (30.0) | (30.2) | (33.5) |
| Other Expenses | (51.2) | (50.5) | (49.8) | (49.1) | (48.1) | (47.3) | (47.5) | (47.7) | (48.0) | (48.3) | (48.7) | (49.0) | (81.0) |
| PFI Operating Expenses | (12.8) | (13.3) | (13.6) | (13.7) | (14.1) | (14.6) | (15.0) | (15.5) | (16.1) | (16.3) | (16.7) | (17.3) | (0.0) |
| Total Operating Expenditure | (384.4) | (391.0) | (390.8) | (390.7) | (389.7) | (390.0) | (395.5) | (400.1) | (404.7) | (410.6) | (416.9) | (423.3) | (537.3) |
| EBITDA | (18.8) | 16.6 | 23.9 | 27.7 | 27.7 | 27.9 | 28.2 | 30.0 | 31.8 | 32.5 | 32.9 | 33.3 | 38.1 |
| EBITDA Margin (%) | (5.1%) | 4.1% | 5.8% | 6.6% | 6.6% | 6.7% | 6.7% | 7.0% | 7.3% | 7.3% | 7.3% | 7.3% | 6.6% |
| Gain/(loss) on asset disposals | (0.0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Impairment Losses (Reversals) net | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Depreciation & Amortisation | (11.7) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) | (11.5) |
| Interest / Contingent Rent | (10.4) | (11.6) | (12.2) | (12.9) | (13.3) | (13.7) | (14.0) | (14.2) | (14.5) | (14.8) | (15.0) | (15.2) | (0.0) |
| Interest payable on Loans | (2.4) | (3.2) | (3.3) | (3.0) | (2.6) | (2.5) | (2.4) | (2.3) | (2.2) | (2.1) | (2.0) | (1.9) | (1.0) |
| PDC Dividend | 0.0 | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.1) | (0.4) | (0.7) | (6.4) |
| Other Non-Operating | 0.3 | 0.0 | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) |
| Total Non-operating | (24.2) | (26.3) | (27.2) | (27.6) | (27.6) | (27.8) | (28.0) | (28.2) | (28.4) | (28.7) | (29.1) | (29.4) | (19.1) |
| Net Surplus / (Deficit) | (43.0) | (9.6) | (3.3) | 0.1 | 0.1 | 0.1 | 0.2 | 1.8 | 3.4 | 3.8 | 3.9 | 3.9 | 19.0 |
| Net Surplus / (Deficit) margin (%) | (12%) | (2%) | (1%) | 0% | 0% | 0% | 0% | 0% | 1% | 1% | 1% | 1% | 3% |
| Normalised (excluding impairments / Disposals) | (43.0) | (9.6) | (3.3) | 0.1 | 0.1 | 0.1 | 0.2 | 1.8 | 3.4 | 3.8 | 3.9 | 3.9 | 19.0 |
10.8.2 Option A – Business As Usual
The financial deficit position of the Trust improves from the current FY19 deficit of £43.0m as a consequence of national funding for Provider Sustainability Fund (PSF), Financial Recovery Fund (FRF) Marginal Rate Emergency Tariff (MRET). This alongside the delivery of CIP sees the Trust return to financial surplus in FY22 and return to financial surplus without national non-recurrent FRF funding in FY25. The total required FRFvunder the Business As Usual is £52.7m (FY21-FY24) compared with £72m (FY21-FY26).
The financial modelling for the Business As Usual option is financially favourable as the Trust would return to financial balance without FRF two years earlier, in FY25 compared with FY27 under the Agreed Option. The key driver for this is the non-recurrent costs required to deliver the service reconfiguration, increased PDC charges under the Agreed Option to support the investment into the estate and the associated depreciation charge on this investment.
The financial modelling does not reflect the estate and service risk that the Trust would be carrying in the short-medium term as within the Business As Usual modelling the estate does not receive any investment to address the £95m backlog maintenance. This risk is unsustainable and therefore the investment within the Agreed Option is required.
10.8.3 Impact on the Statement of Comprehensive Income (incremental) – Agreed vs. Business As Usual
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Revenue (Excluding PSF / FRF) | 0.0 | 0.0 | 0.0 | 0.0 | (0.0) | 0.0 | (0.2) | 0.1 | 0.5 | 0.9 | 0.9 | 0.9 | 1.5 |
| PSF / FRF | 0.0 | 0.0 | 0.0 | 0.8 | 2.3 | 4.7 | 9.4 | 2.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Revenue costs | |||||||||||||
| Employee Benefit Expenses | 0.0 | 0.0 | 0.0 | (0.3) | (0.5) | (1.1) | (4.6) | 3.4 | 6.9 | 10.1 | 10.0 | 9.9 | 7.8 |
| Drugs | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.3 | 0.3 | 0.3 | 0.2 | 0.2 | (0.3) |
| Clinical Supplies & Services | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.3 | 0.3 | 0.2 | 0.2 | 0.2 | (0.3) |
| Other Expenses | 0.0 | 0.0 | 0.0 | 0.0 | (1.0) | 0.0 | 0.3 | 0.6 | 0.9 | 1.3 | 1.2 | 1.2 | 0.8 |
| PFI Operating Expenses | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Revenue Costs | 0.0 | 0.0 | 0.0 | (0.3) | (1.5) | (1.1) | (3.8) | 4.5 | 8.4 | 11.9 | 11.7 | 11.5 | 8.1 |
| Gain/(loss) on asset disposals | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Impairment Losses (Reversals) net | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | (26.5) | (16.3) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Depreciation & Amortisation | 0.0 | 0.0 | (0.1) | (0.3) | (0.5) | (0.6) | (0.6) | (3.8) | (3.8) | (3.8) | (3.8) | (3.8) | (3.8) |
| Interest / Contingent Rent on PFI leases & liabilities | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Interest payable on Loans | 0.0 | 0.0 | (0.1) | (0.2) | (0.1) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | (0.0) |
| PDC Dividend | 0.0 | 0.0 | 0.0 | 0.0 | (0.3) | (3.0) | (5.0) | (4.8) | (4.3) | (4.6) | (4.8) | (4.9) | (5.9) |
| Other Non-Operating | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Non-Operating Costs | 0.0 | 0.0 | (0.1) | (0.5) | (0.9) | (3.6) | (32.0) | (24.9) | (8.1) | (8.4) | (8.6) | (8.7) | (9.8) |
| Incremental impact on I&E surplus/ (deficit) | 0.0 | 0.0 | (0.1) | 0.0 | (0.0) | (0.0) | (26.6) | (18.0) | 0.8 | 4.3 | 4.0 | 3.7 | (0.2) |
| less Impairments | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 26.5 | 16.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| less Non-recurrent costs | 0.0 | 0.0 | 0.3 | 0.5 | 2.1 | 6.9 | 0.2 | ||||||
| Incremental impact on I&E surplus / (deficit) | 0.0 | 0.0 | 0.2 | 0.5 | 2.1 | 6.9 | 0.0 | (1.7) | 0.8 | 4.3 | 4.0 | 3.7 | (0.2) |
10.8.4 Impact on Cash Flow (incremental) – Agreed vs. Business as Usual
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Capital costs | 0.0 | 0.0 | (8.1) | (6.0) | (49.3) | (86.6) | (45.5) | (4.2) | (4.2) | (4.2) | (4.2) | (4.2) | (3.8) |
| Revenue costs (excl Depreciation) | 0.0 | 0.0 | (0.1) | 0.3 | 0.5 | 0.6 | 0.4 | 2.1 | 4.6 | 8.1 | 7.8 | 7.5 | 3.6 |
| PWLB Capital Loan | 0.0 | 0.0 | 8.0 | 6.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Revenue Support Loan | 0.0 | 0.0 | 0.2 | 0.3 | 0.8 | 1.6 | 3.3 | 0.8 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| PFI Finance | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| PDC | 0.0 | 0.0 | 0.0 | 0.0 | 66.4 | 85.6 | 44.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Loan repayments | 0.0 | 0.0 | 0.0 | (0.3) | (16.8) | (0.4) | (1.2) | (2.9) | (0.4) | 0.4 | 0.4 | 0.4 | (0.0) |
| PFI Lease repayments | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Incremental impact on Cash | 0.0 | 0.0 | 0.1 | 0.3 | 1.7 | 0.8 | 1.5 | (4.2) | 0.0 | 4.3 | 4.0 | 3.7 | (0.2) |
| Cumulative impact on Cash Flow | 0.0 | 0.0 | 0.1 | 0.4 | 2.0 | 2.8 | 4.3 | 0.1 | 0.1 | 4.4 | 8.4 | 12.1 | 40.9 |
10.8.5 Statement of financial position (incremental) – Agreed vs. Business as Usual
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Property plant and equipment | 0.0 | 0.0 | 8.0 | 14.0 | 62.4 | 148.0 | 166.1 | 129.2 | 129.2 | 129.2 | 129.2 | 129.2 | 129.2 |
| Cash and cash equivalents | 0.0 | 0.0 | 0.1 | 0.1 | 1.2 | 1.2 | 1.0 | (0.7) | 0.1 | 4.4 | 8.4 | 12.1 | 40.9 |
| Loans | 0.0 | 0.0 | (8.2) | (14.2) | 1.8 | 0.5 | (1.5) | 0.6 | 1.0 | 0.6 | 0.2 | (0.2) | (0.1) |
| PFI Lease | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Taxpayers Equity | 0.0 | 0.0 | (0.1) | 0.2 | 66.2 | 151.4 | 168.9 | 129.9 | 130.3 | 134.2 | 137.8 | 141.1 | 170.0 |
10.9 Detailed Financial Expenditure – Affordability (Option B – Do Minimum)
For comparison, the activity, workforce and capital plans for the Existing Model Option are modelled within the financial expenditure table below:
10.9.1 Income and Expenditure Account
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Clinical Revenue | 319.3 | 332.7 | 345.4 | 352.2 | 359.3 | 366.6 | 374.2 | 379.9 | 385.7 | 391.8 | 397.9 | 404.1 | 512.2 |
| Non Protected/Non Mandatory Clinical Revenue | 7.3 | 6.2 | 6.3 | 6.5 | 6.6 | 6.8 | 6.9 | 7.1 | 7.3 | 7.4 | 7.6 | 7.8 | 11.0 |
| Other Revenue | 39.0 | 40.5 | 40.9 | 41.3 | 41.7 | 42.1 | 42.5 | 43.0 | 43.4 | 43.8 | 44.3 | 44.7 | 51.9 |
| PSF / FRF | 28.3 | 22.1 | 18.7 | 10.4 | 3.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Total Revenue | 365.6 | 407.6 | 414.7 | 418.7 | 418.1 | 418.8 | 423.7 | 430.0 | 436.4 | 443.0 | 449.7 | 456.6 | 575.1 |
| Employee Benefit Expenses | (253.3) | (259.5) | (260.4) | (261.5) | (261.9) | (263.0) | (267.0) | (271.0) | (275.2) | (280.5) | (285.9) | (291.5) | (385.2) |
| Drugs | (37.2) | (38.1) | (37.5) | (37.0) | (36.4) | (35.8) | (35.5) | (35.2) | (34.8) | (34.6) | (34.5) | (34.3) | (31.5) |
| Clinical Supplies & Services | (30.0) | (29.5) | (29.4) | (29.4) | (29.3) | (29.2) | (29.3) | (29.4) | (29.5) | (29.7) | (29.9) | (30.1) | (33.0) |
| Other Expenses | (51.2) | (50.5) | (49.8) | (49.1) | (48.1) | (47.3) | (47.4) | (47.6) | (47.8) | (48.2) | (48.5) | (48.9) | (80.5) |
| PFI Operating Expenses | (12.8) | (13.3) | (13.6) | (13.7) | (14.1) | (14.6) | (15.0) | (15.5) | (16.1) | (16.3) | (16.7) | (17.3) | (0.0) |
| Total Operating Expenditure | (384.4) | (391.0) | (390.8) | (390.7) | (389.7) | (390.0) | (394.2) | (398.8) | (403.4) | (409.3) | (415.5) | (422.0) | (530.2) |
| EBITDA | (18.8) | 16.6 | 23.9 | 28.1 | 28.4 | 28.8 | 29.5 | 31.2 | 33.0 | 33.7 | 34.2 | 34.6 | 44.9 |
| EBITDA Margin (%) | (5.1%) | 4.1% | 5.8% | 6.67% | 6.8% | 6.9% | 7.0% | 7.3% | 7.6% | 7.6% | 7.6% | 7.6% | 7.8% |
| Gain/(loss) on asset disposals | (0.0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Impairment Losses (Reversals) net | 0.0 | 0.0 | (0.9) | (0.9) | (0.9) | (0.9) | (0.9) | (0.9) | (0.9) | (0.9) | (0.9) | (0.9) | 0.0 |
| Total Depreciation & Amortisation | (11.7) | (11.5) | (11.5) | (11.7) | (11.8) | (12.0) | (12.1) | (12.3) | (12.4) | (12.6) | (12.7) | (12.9) | (13.0) |
| Interest / Contingent Rent | (10.4) | (11.6) | (12.2) | (12.9) | (13.3) | (13.7) | (14.0) | (14.2) | (14.5) | (14.8) | (15.0) | (15.2) | (0.0) |
| Interest payable on Loans | (2.4) | (3.2) | (3.4) | (3.2) | (3.0) | (3.0) | (3.0) | (3.0) | (3.1) | (3.1) | (3.1) | (3.1) | (1.4) |
| PDC Dividend | 0.0 | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (0.3) | (0.6) | (8.1) |
| Other Non-Operating | 0.3 | 0.0 | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) | (0.2) |
| Total Non-operating | (24.2) | (26.3) | (28.2) | (28.9) | (29.2) | (29.6) | (30.1) | (30.6) | (31.1) | (31.5) | (32.2) | (32.8) | (22.6) |
| Net Surplus / (Deficit) | (43.0) | (9.6) | (4.3) | (0.8) | (0.8) | (0.8) | (0.7) | 0.6 | 2.0 | 2.2 | 2.0 | 1.9 | 22.3 |
| Net Surplus / (Deficit) margin (%) | (12%) | (2%) | (1%) | (0%) | (0%) | (0%) | (0%) | 0% | 0% | 0% | 0% | 0% | 4% |
| Normalised (excluding impairments / Disposals) | (43.0) | (9.6) | (3.4) | 0.1 | 0.1 | 0.1 | 0.2 | 1.8 | 3.4 | 3.8 | 3.9 | 3.9 | 19.0 |
10.9.2 Option B – Do Minimum
The financial deficit position of the Trust improves from the current FY19 deficit of £43.0m as a consequence of national funding for Provider Sustainability Fund (PSF), Financial Recovery Fund (FRF) Marginal Rate Emergency Tariff (MRET). This alongside the delivery of CIP sees the Trust return to financial surplus in FY22 and return to financial surplus without national non-recurrent FRF funding in FY25. The total required FRF under the Business As Usual is £52.7m (FY21-FY24) compared with £72m (FY21-FY26).
The financial modelling for the Business As Usual option is financially favourable as the Trust would return to financial balance without FRF two years earlier, in FY25 compared with FY27 under the Agreed Option. The key driver for this is the non-recurrent costs required to deliver the service reconfiguration, increased PDC charges under the Agreed Option to support the investment into the estate and the associated depreciation charge on this investment.
The financial modelling does not reflect the estate and service risk that the Trust would be carrying in the short-medium term as within the Business As Usual modelling the estate does not receive any investment to address the £95m backlog maintenance. This risk is unsustainable and therefore the investment within the Agreed Option is required.
10.9.3 Impact on the Statement of Comprehensive Income (incremental) – Agreed vs. Do Minimum
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Revenue (Excluding PSF / FRF) | 0.0 | 0.0 | 0.0 | (0.0) | 0.0 | (0.0) | (0.1) | 0.2 | 0.6 | 0.9 | 1.0 | 1.0 | 1.8 |
| PSF / FRF | 0.0 | 0.0 | 0.0 | 0.4 | 1.7 | 3.7 | 9.4 | 2.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Revenue costs | |||||||||||||
| Employee Benefit Expenses | 0.0 | 0.0 | 0.0 | (0.3) | (0.5) | (1.1) | (5.6) | 2.4 | 6.0 | 9.1 | 9.0 | 8.9 | 2.1 |
| Drugs | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | (0.7) |
| Clinical Supplies & Services | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | (0.8) |
| Other Expenses | 0.0 | 0.0 | 0.0 | 0.0 | (1.0) | 0.0 | 0.2 | 0.5 | 0.8 | 1.1 | 1.1 | 1.1 | 0.3 |
| PFI Operating Expenses | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Revenue Costs | 0.0 | 0.0 | 0.0 | (0.3) | (1.5) | (1.1) | (5.1) | 3.2 | 7.1 | 10.5 | 10.3 | 10.1 | 1.0 |
| Gain/(loss) on asset disposals | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Impairment Losses (Reversals) net | 0.0 | 0.0 | 0.9 | 0.9 | 0.9 | 0.9 | (25.6) | (15.4) | 0.9 | 0.9 | 0.9 | 0.9 | 0.0 |
| Total Depreciation & Amortisation | 0.0 | 0.0 | (0.1) | (0.2) | (0.2) | (0.1) | 0.0 | (3.1) | (2.9) | (2.8) | (2.6) | (2.5) | (2.3) |
| Interest / Contingent Rent on PFI leases & liabilities | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Interest payable on Loans | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.5 | 0.6 | 0.7 | 0.9 | 1.0 | 1.1 | 1.2 | 0.4 |
| PDC Dividend | 0.0 | 0.0 | 0.0 | 0.0 | (0.3) | (3.0) | (5.0) | (4.8) | (4.3) | (4.7) | (4.8) | (5.0) | (4.3) |
| Other Non-Operating | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total Non-Operating Costs | 0.0 | 0.0 | 0.8 | 0.8 | 0.7 | (1.8) | (29.9) | (22.6) | (5.5) | (5.6) | (5.5) | (5.4) | (6.2) |
| Incremental impact on I&E surplus/ (deficit) | 0.0 | 0.0 | 0.8 | 0.9 | 0.9 | 0.9 | (25.7) | (16.9) | 2.2 | 5.9 | 5.8 | 5.8 | (3.5) |
| less Impairments | 0.0 | 0.0 | (0.9) | (0.9) | (0.9) | (0.9) | 25.6 | 15.4 | (0.9) | (0.9) | (0.9) | (0.9) | 0.0 |
| less Non-recurrent costs | 0.0 | 0.0 | 0.3 | 0.5 | 2.1 | 6.9 | 0.2 | ||||||
| Incremental impact on I&E surplus / (deficit) | 0.0 | 0.0 | 0.2 | 0.5 | 2.1 | 6.9 | 0.1 | (1.4) | 1.3 | 5.0 | 4.9 | 4.9 | (3.5) |
10.9.4 Impact on Cash Flow (incremental) – Agreed vs. Do Minimum
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Capital costs | 0.0 | 0.0 | (2.1) | (0.1) | (43.5) | (80.8) | (39.9) | 1.3 | 1.2 | 1.1 | 1.1 | 1.0 | (4.7) |
| Revenue costs (excl Depreciation) | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 0.1 | (0.2) | 1.6 | 4.2 | 7.8 | 7.5 | 7.3 | (1.2) |
| PWLB Capital Loan | 0.0 | 0.0 | 2.0 | 0.0 | (6.0) | (6.0) | (6.0) | (6.0) | (6.0) | (6.0) | (6.0) | (6.0) | 0.0 |
| Revenue Support Loan | 0.0 | 0.0 | 0.1 | 0.1 | 0.6 | 1.3 | 3.3 | 0.8 | 0.0 | 0.0 | 0.0 | 0.0 | (0.0) |
| PFI Finance | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| PDC | 0.0 | 0.0 | 0.0 | 0.0 | 66.4 | 85.6 | 44.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Loan repayments | 0.0 | 0.0 | 0.0 | (0.1) | (16.1) | 0.5 | 0.1 | (1.7) | 1.1 | 2.1 | 2.3 | 2.6 | 2.4 |
| PFI Lease repayments | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Incremental impact on Cash | 0.0 | 0.0 | (0.0) | 0.1 | 1.5 | 0.7 | 1.8 | (3.9) | 0.5 | 5.0 | 4.9 | 4.9 | (3.5) |
| Cumulative impact on Cash Flow | 0.0 | 0.0 | (0.0) | 0.1 | 1.7 | 2.4 | 4.2 | 0.3 | 0.8 | 5.8 | 10.7 | 15.5 | 28.0 |
10.9.5 Statement of financial position (incremental) – Agreed vs. Do Minimum
| £m | FY19 | FY20 | FY21 | FY22 | FY23 | FY24 | FY25 | FY26 | FY27 | FY28 | FY29 | FY30 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yr 0 | Yr 1 | Yr 2 | Yr 3 | Yr 4 | Yr 5 | Yr 6 | Yr 7 | Yr 8 | Yr 9 | Yr 10 | Yr 25 | ||
| Property plant and equipment | 0.0 | 0.0 | 2.9 | 3.8 | 47.1 | 127.6 | 140.6 | 98.6 | 93.5 | 88.4 | 83.5 | 78.2 | 78.2 |
| Cash and cash equivalents | 0.0 | 0.0 | 0.1 | 0.1 | 1.1 | 1.0 | 0.8 | (0.6) | 0.7 | 5.7 | 10.6 | 15.4 | 27.9 |
| Loans | 0.0 | 0.0 | (2.1) | (2.1) | 19.4 | 23.6 | 26.3 | 33.2 | 38.1 | 42.0 | 45.7 | 49.1 | 13.2 |
| PFI Lease | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Taxpayers Equity | 0.0 | 0.0 | 0.8 | 1.8 | 68.2 | 153.6 | 171.0 | 132.0 | 132.4 | 136.2 | 139.7 | 142.9 | 119.4 |
10.10 Financial Affordability Conclusion
The table below provides a comparison of the affordability compared to the Existing Service Model position.
10.10.1 Income and Expenditure Business As Usual vs. Agreed Option
| £m | FY27 | FY27 | FY27 | FY27 | FY27 | FY45 | FY45 | FY45 | FY45 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|
| Business As Usual | Do Minimum | Agreed | Business As Usual Variance | Do Minimum Variance | Business As Usual | Do Minimum | Agreed | Business As Usual Variance | Do Minimum Variance | |
| Option A | Option B | Option C | Option A | Option B | Option C | |||||
| £m | £m | £m | £m | £m | £m | £m | £m | £m | £m | |
| Total Revenue | 436.5 | 436.4 | 437.0 | 0.5 | 0.6 | 575.4 | 575.1 | 576.9 | 1.5 | 1.8 |
| Total Operating Expenditure | (404.7) | (403.4) | (396.2) | 8.4 | 7.1 | (537.3) | (530.2) | (529.2) | 8.1 | 1.0 |
| EBITDA | 31.8 | 33.0 | 40.7 | 8.9 | 7.7 | 38.1 | 44.9 | 47.7 | 9.5 | 2.7 |
| Total Non-operating Expenses | (28.4) | (31.1) | (36.5) | (8.1) | (5.5) | (19.1) | (22.6) | (28.9) | (9.8) | (6.2) |
| Net Surplus / (Deficit) | 3.4 | 2.0 | 4.2 | 0.8 | 2.2 | 19.0 | 22.3 | 18.8 | (0.2) | (3.5) |
| Net Surplus / (Deficit) margin (%) | 0.0 | 0.0 | 0.0 | 0.2% | 0.5% | 3.3% | 3.9% | 3.3% | 0.0% | -0.6% |
| FY27 Cumulative normalised Surplus / (Deficit) | (50.2) | (51.0) | (41.4) | 8.8 | 9.6 | |||||
| FY45 Cumulative normalised Surplus / (Deficit) | 97.3 | 115.1 | 131.9 | 34.7 | 16.8 |
10.10.2 Statement of Financial Position Business As Usual and Do Minimum vs. Agreed Option
| £m | FY27 | FY27 | FY27 | FY27 | FY27 | FY45 | FY45 | FY45 | FY45 | FY45 |
|---|---|---|---|---|---|---|---|---|---|---|
| Business As Usual | Do Minimum | Agreed | Business As Usual Variance | Do Minimum Variance | Business As Usual | Do Minimum | Agreed | Business As Usual Variance | Do Minimum Variance | |
| Option A | Option B | Option C | Option A vs.Option C | Option B vs. Option C | Option A | Option B | Option C | Option A vs. Option C | Option B vs. Option C | |
| £ | £ | £ | £ | £m | £m | £m | £m | £m | £m | |
| Property, Plant and Equipment | 233.4 | 269.1 | 362.6 | 129.2 | 93.5 | 230.5 | 281.5 | 359.7 | 129.2 | 78.2 |
| Current Assets | 37.5 | 36.9 | 37.6 | 0.1 | 0.7 | 94.4 | 107.4 | 135.3 | 40.9 | 27.9 |
| Total Assets | 270.9 | 306.0 | 400.2 | 129.3 | 94.2 | 324.8 | 388.8 | 494.9 | 170.1 | 106.1 |
| Current Liabilities | (46.4) | (47.3) | (46.3) | 0.1 | 1.1 | (43.1) | (43.6) | (43.0) | 0.1 | 0.6 |
| Non-Current Liabilities | (205.8) | (242.0) | (204.9) | 0.9 | 37.1 | (67.6) | (80.4) | (67.8) | (0.2) | 12.6 |
| Total Liabilities | (252.1) | (289.3) | (251.2) | 1.0 | 38.2 | (110.7) | (124.1) | (110.8) | (0.1) | 13.3 |
| Net Assets employed | 18.8 | 16.7 | 149.1 | 130.3 | 132.4 | 214.1 | 264.7 | 384.1 | 170.0 | 119.4 |
| Public dividend capital | 120.1 | 120.1 | 316.6 | 196.5 | 196.5 | 120.1 | 120.1 | 316.6 | 196.5 | 196.5 |
| Retained Earnings (Accumulated Losses) | (163.8) | (171.0) | (207.9) | (44.1) | (36.9) | (16.4) | (7.5) | (34.5) | (18.2) | (27.0) |
| Revaluation reserve | 62.5 | 67.5 | 40.3 | (22.2) | (27.2) | 110.4 | 152.2 | 102.0 | (8.4) | (50.2) |
| Total taxpayers’ equity | 18.8 | 16.7 | 149.1 | 130.3 | 132.4 | 214.1 | 264.7 | 384.1 | 170.0 | 119.4 |
10.10.3 Funding Requirements Business As Usual and Do Minimum vs. Agreed Option
| £m | FY45 | FY45 | FY45 | FY45 | FY45 |
|---|---|---|---|---|---|
| Business As Usual | Do Minimum | Agreed Option | Business As Usual Variance | Do Minimum Variance | |
| Option A | Option B | Option C | |||
| PWLB Capital Loan | 0.0 | (13.2) | 0.0 | (0.0) | 13.2 |
| Revenue Support Loan | (64.5) | (64.6) | (64.6) | (0.1) | (0.0) |
| Emergency Capital | (2.6) | (2.6) | (2.6) | 0.0 | 0.0 |
| PDC funding | 0.0 | 0.0 | (196.5) | (196.5) | (196.5) |
| Total funding requirement | (67.1) | (80.4) | (263.7) | (196.4) | (£183.3) |
The funding requirement analysis outlines that the Agreed option requires additional funding of £196.5m, received as PDC, offset by reduced PWLB capital loan.
Additional revenue loans only required for 2 years from FY20 in all cases due to assumed FRF returning the Trust to financial surplus in FY22 in all cases. Any other borrowing is for timing of cash flow as FRF is received quarterly in arrears and in line with a working capital loan and is repaid on receipt of the FRF funding.
The net cost of the investment is £196.4m when compared to the Business As Usual case and £183.4m compared to the Do Minimum case at FY45.
10.11 Conclusions of the Financial Case
It is concluded that Option C is the favourable option. The Agreed Service Option demonstrates overall affordability for the investment and enables the Trust to deliver additional financial efficiencies.
The financial plan demonstrates that savings enabled through reconfiguration present a favourable case compared to the Business As Usual and Do Minimum. Downside scenarios test the sensitivity of the plan however the Trust retains overall affordability within the financial plan. Potential upside sensitivities offer the Trust the opportunity to return to financial balance in FY22 years and reduces the required Financial Recovery Fund monies by £19.2m to FY26.
The modelled clinical activity and revenue has been agreed as affordable for the local health sector, with the Trusts key commissioners outlining that the plans are affordable. The CIP is consistent with the national efficiency requirements reflecting assumptions of cost inflation and price deflation. The additional investment in the estate enables greater efficiencies to be realised in years FY26-FY28 through greater operational efficiency and transformation.
11. Management Case
The purpose of this section is to describe the systems and processes that will be established to ensure the successful implementation of the proposed option for the configuration of the Trust’s hospital services. This is structured across the following key areas:
- • Programme management and governance - how the programme will be managed including reporting and accountability arrangements and the use of special advisors
- • Programme Timeline - the key phases of work and the programme timeline
- • Risk Management - the approach to management of risk and the risk register
- • Benefits Realisation and Post Project Evaluation - arrangements for ongoing review of benefits.
11.1 Management and Governance
The Trust’s management and governance of the programme will be aligned with best practice described in the Treasury recommended methodology for programme management i.e. Managing Successful Programmes (MSP). The over-arching programme management will focus on the delivery of the key financial and non-financial benefits and outcomes associated with the reconfiguration of hospital services.
PRINCE 2 project methodology will be used to manage underpinning project life cycles from start-up to closure to ensure project planning and monitoring are carried out rigorously. The project management will focus on delivery of the key enabling actions and outputs that support achievement of the overarching programme benefits and outcomes.
Subject to Treasury approval to implement the FBC an Integrated Assurance and Approval Plan (IAAP) will be developed. This will detail the planning, coordination and provision of assurance activities and Treasury approval points (gateways) throughout the programme.
11.1.1 Governance Structure
The following diagram provides an overview of the programme structure. The structure is designed to ensure there is one overall Senior Responsible Owner, one Programme Director and one Programme Manager each with the required authority and responsibility to manage the programme on behalf of the Trust. The programme structure is explained in more detail below.
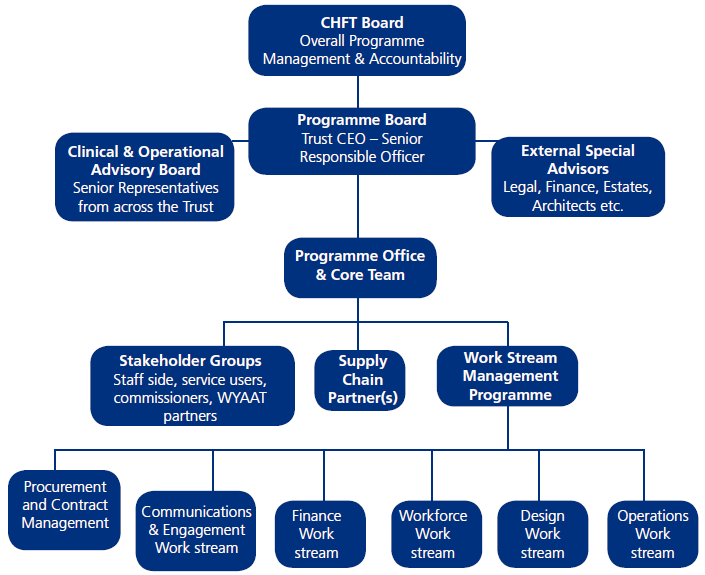
CHFT Board will have overall responsibility and accountability for the programme ensuring that the project has a viable and affordable business case that will deliver value for money and best quality healthcare through effective management of the procurement process and implementation of the proposed configuration of services. The Board will seek assurance from the Senior Responsible Owner and Programme Board on any aspect of the programme that may pose a risk to successfully achieving the investment objectives and realisation of the expected benefits.
The Programme Board will be chaired by an independent chair. The Chief Executive of CHFT will be the Senior Responsible Owner (SRO) and will lead the programme implementation. The Programme Board will have Non-Executive and Executive Directors (including the Programme Director) as members and also include representation from Trust senior clinicians, Calderdale and Huddersfield Solutions Ltd (CHS) and external specialist / technical advisors. Representatives from NHSE, NHSI, DH, CCGs and the West Yorkshire and Harrogate Health and Care Partnership will be invited to be members of the Programme Board as well as two patient representatives.
The Programme Board will approve and manage the programme plan and sign off the key outputs and decisions at each stage of the project including:
- Patient and staff communications and engagement;
- The competitive dialogue process and procurement;
- Review of all the key deliverables and the activities required to deliver them;
- The activities required to validate the quality of the deliverables;
- The resources and time needed for all activities and any need for people with specific capabilities and competencies;
- The dependencies between activities and any associated constraints when activities will occur;
- The points at which progress will be monitored, controlled and reviewed;
- The provision of regular reports, updates and assurance to CHFT Board, NHSI and Treasury;
- Maintenance of a detailed risk register and mitigation of risk factors affecting the successful delivery of the project;
- Maintenance of a benefits realisation register and monitoring of delivery;
- Considering and recommending to the Trust Board any changes to the project scope, budget or timescale if required;
- Review of serious issues, which have reached threshold level;
- Broker relationships with stakeholders within and outside the project to maintain positive support for the programme;
- Maintain awareness of the broader strategic perspective advising the SRO on how it may affect the project.
Specialist Advisors – implementation of the proposed configuration will require a complex programme of work and the Trust will secure the necessary external specialist expertise and advice that is required. This will include, for example: legal, procurement, project management, private finance, estates, architects, health planning, facilities management, equipping, town planning, engineering, traffic and transport, quantity surveying, life cycle analysis, health and safety etc. The external advisors will provide advice to the SRO, the Programme Director, the Programme Board, and the Trust Board and will advise and inform work undertaken by the project work stream groups. The Trust will also appoint internal ‘Clinical Subject Matter Experts’ in key areas to inform the work of the programme, this will provide dedicated time of clinical staff to inform the development and will cover areas such as emergency and urgent care, acute inpatient medical care, planned surgery, paediatric services, maternity services, outpatient services.
Clinical and Operational Advisory Board – this will be a clinical and operational leadership committee comprising senior representatives of the Clinical Divisions who manage the operational services of the Trust; General Practice doctors; Directors of Social Care; and Executive Directors (DoN, MD, COO). They will provide leadership within the organisation to ensure successful delivery of the project and assurance to the Programme Board and the Trust Board about the project. The group will provide guidance to the Project Director and ensure that Trust operational resources will be available to support the project. The group will:
- Provide leadership, mandate and focus within the Trust ensuring that clinical objectives inform and drive effective delivery of the competitive dialogue process;
- Provide advice to the Programme Director, Programme Board and Trust Board, raising any concerns and providing expert opinion to support decision making;
- Support resolution of issues at organisational level when required;
- Support resolution of issues which impact on the Trust involving senior external stakeholders, the press; Government, arm’s length bodies etc.;
- Provide assessment of serious issues;
- Ensure that project plans are achievable and facilitate delivery as required;
- Review the risk register on a quarterly basis and / or at key milestones and advise the Programme Board prior to approval and help to mitigate risks at organisational level.
The Programme Office and Core Team will be led by the Programme Director and proactively drive delivery of the programme plan and critical path. It will provide programme management support to the work streams and will be responsible for the management of all programme management processes, including preparing and managing papers for governance arrangements, proactive risk and issue management and progress reporting. The programme office will have sufficient resource capability and capacity available to effectively support the programme, recognising the scale, complexity and likely fast-paced nature of the programme. This will include a core team within the programme office with the necessary skills for:
- Planning and delivering the Competitive Dialogue and bid evaluation process and all other activities to financial close;
- Developing, maintaining and implementing project plans;
- Co-ordinating working groups and evaluation teams as required;
- Monitoring progress and reporting to the Programme Board and the Clinical and Operational Advisory Board;
- Managing issues as they arise in line with the issue management policy and escalating those above threshold to the Programme Board;
- Managing change control;
- Managing project advisors, ensuring that their contribution is well understood and that the Trust obtains best advice and value;
- Managing risks in line with project risk management strategy;
- Ensuring effective development and delivery of the Engagement and Communications Plan.
Key Stakeholder Groups – the programme office and core team will proactively work to ensure the engagement, involvement and coordination of key stakeholder groups input to the programme. Significant communication and engagement has taken place over the last two years. The programme will continue actively engaging with stakeholders through the next phases and during implementation. This will include for example:
- Calderdale and Kirklees Health and Wellbeing Boards – ensuring that implementation of the proposed changes are aligned with Health and Wellbeing Board’s plans of how best to meet the needs of their local population and tackle local inequalities in health.
- Calderdale and Kirklees Joint Health Scrutiny Committee – ensuring continued public scrutiny through the period of implementation.
- Greater Huddersfield and Calderdale CCGs – ensuring that clinical commissioners are fully involved and informed of the implementation plans and progress.
- CHFT Council of Governors – ensuring that Governors are well informed about what changes are proposed and able to contribute and have a say in how they are to be delivered.
- Patients, Public and local Healthwatch – ensuring that patients are well informed about what changes are proposed, have a say in how they are to be delivered and, ultimately, are fully aware of which services will be delivered from which locations in the future.
- Other Providers – communication and involvement of other providers that are impacted by the changes and/or are critical to implementation (e.g. voluntary sector organisations, ambulance services, mental health, primary care, WYAAT and neighbouring acute hospitals, the existing CRH PFI provider).
- NHS staff – actively engaging with staff to ensure they are fully aware of the implementation plans and able to contribute to the plans promoting their central role in making these changes happen.
- Clinicians – will be actively involved in the planning and implementation of service change to ensure patient safety is not compromised as changes are made.
- Local Authorities – work with partners in social care to co-design and begin to deliver the transformation to Out of Hospital services which is critical to the success of the reconfiguration programme.
- West Yorkshire and Harrogate Health and Care Partnership – work to ensure the implementation of the proposed changes fit with West Yorkshire overall strategy for the development of better health and care services for West Yorkshire and Harrogate as a whole.
As part of the programme design and mobilisation phase the stakeholder engagement plan will be updated to provide a comprehensive view of planned events and activities throughout implementation.
Supply Chain Partner(s) – the success of the programme is reliant on effective supply chain partner(s) that will provide estates solutions to enable implementation of the proposed configuration of hospital services. The Programme Office and Core Team will, in accordance, with the ‘partnering’ principle, ensure there are regular meetings between senior managers in the Trust and supplier organisation(s). These meetings will formally monitor and report to the Programme Board the service streams and outputs which are being contracted for and progress against the implementation timescales which have been agreed for their delivery.
As described in section 9.1 the Trust’s preferred approach at this stage is to instruct Calderdale Health Solutions (CHS) to act on behalf of the Trust to deliver the necessary procurement(s) and subsequent contract management of suppliers to deliver the estate capital development works. CHS is a wholly owned subsidiary of the Trust and provides a fully managed suite of healthcare facilities for use by CHFT and provides value to CHFT through its specific service offering and through its ability to manage developments and operational risk for the Trust and other parties. CHS’s status as a “Teckal” trading company means that the Trust is able to contract directly with CHS without the need for a competitive procurement process. This approach will be further defined in the Outline Business Case.
Project work streams will have a senior sponsor who will also be a member of the Programme Board. Whilst the sponsor will remain accountable for the work stream, it is expected that they will delegate responsibility for the day-to-day management of, and delivery against, the work stream plan and critical path, to a work stream lead. The Programme Manager (and other members of the Programme Office and Core Team) will support and monitor progress of the work streams against agreed milestones and report this to the Programme Board. The structural chart above shows an example of the range of work streams that may be required. This will vary at different stages of the Programme and other work streams will also be established.
11.1.2 Roles and Responsibilities
The Chief Executive Officer (Senior Responsible Owner for this project), Director of Finance, Medical Director and the Trust’s Chair will ensure strong leadership for the project. The Programme will be supported by a Programme Director and a fully resourced Programme Office and Core Team, of appropriately experienced and qualified individuals. The programme will be managed in line with best practice ensuring that roles and responsibilities are clearly defined. Decision making will be transparent and will be documented to ensure a robust audit trail is maintained.
The Senior Responsible Owner (SRO)
The Chief Executive Officer undertakes the SRO role for this project. The SRO is personally accountable for the success of the project ensuring that the project meets its objectives and delivers benefits. The SRO will ensure that the project maintains business focus in a changing healthcare context and that risks are managed effectively.
The Programme Director
The Programme Director is responsible for day to day decision making on behalf of the SRO and setting high standards for delivery of the project.
The Programme Manager
The Programme Manager will coordinate the activities of the Programme Office and Core Team on a day to day basis and is responsible for ensuring that:
- Procurement and engagement runs smoothly;
- Requests for information, issues and changes are managed appropriately;
- Project standards are maintained;
- Project budget is managed effectively.
The Core Team will meet weekly, or as required, to co-ordinate the work. It reports to the Programme Board.
11.2 Timeline
A high level overview of the programme timeline up to full year ending 2025 (FY25) is shown below. During this period the capital investment and estates build work will be completed enabling the opening of the planned and unplanned hospitals. Full optimisation of the financial and quality benefits associated with the reconfiguration of hospital services will continue beyond year 5. The Trust will continue to programme manage and monitor the realisation of benefits beyond FY25.
11.2.1 High level Project Timeline
Following the DHSC confirmation in December 2018 that capital funding of £196.5m has been allocated to this development it has also been confirmed that approval of a Strategic Outline Case (SOC), Outline Business Case (OBC) and Full Business Case (FBC) by NHS Improvement, DHSC, Ministers and HM Treasury will be required.
The SOC, OBC and FBC will need to be approved by CHFT Trust Board prior to submission to NHS Improvement and letters of support from CCG Governing Bodies, NHS England, and the West Yorkshire & Harrogate Health and Care Partnership Chief Executive will also be required at each stage of approval of the business cases. The content of the SOC, OBC and FBC will take account of Her Majesty’s Treasury (HMT) Green Book guidance on appraisal and evaluation and the supplementary Guide to Developing the Project Business Case (2018) and guidance from NHS Improvement.
Based on these requirements and the associated governance processes, the table below provides an indicative outline timeline for this development. This timeline will require the effective management of existing estate and clinical service risks over this period and is reliant therefore on the assumption that these risks do not escalate at a faster rate. Opportunities to expedite the timeline will also be explored if it is possible to do so whilst ensuring robust governance and stakeholder involvement.
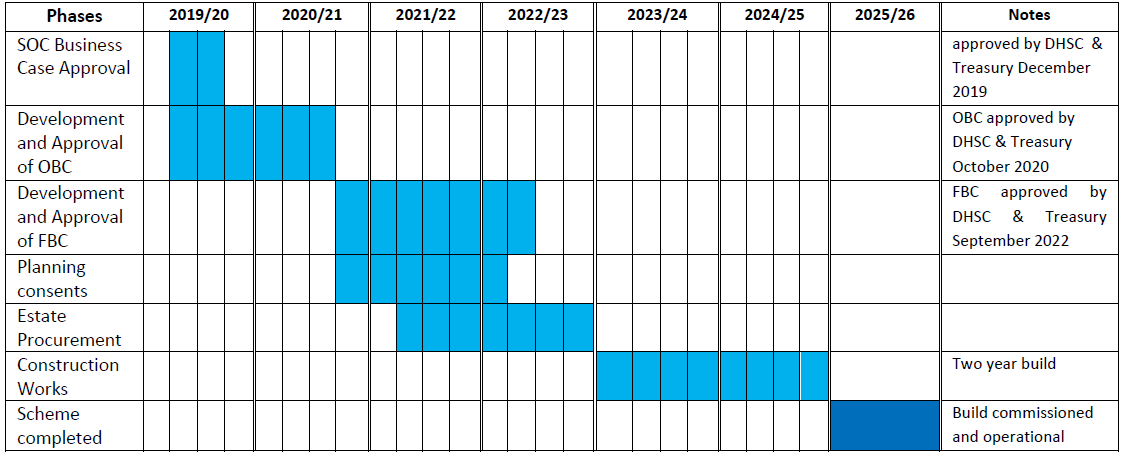
11.3 Risk Management
11.3.1 Programme Risks
The Programme Board will ensure that robust arrangements for the on-going management of risk during the key phases of the programme are established. This will include independent assessment and audit activities. Strategies for the active and effective management of risk will include:
- Identifying possible risks in advance and putting mechanisms in place to minimise the likelihood of them materialising with adverse effects;
- Having rigorous processes in place to monitor the risks, and access to reliable, up to-date
- Information about the risks;
- Having agreed actions to control or mitigate against the adverse consequences of the risks, if they should materialise;
- Ensuring that decision-making processes during the programme are supported by a framework for risk analysis and evaluation.
To identify the specific risks the programme will use a number of approaches that will include:
- Structured review meetings involving the programme board, the clinical and operational advisory board and the programme management team. This will encourage participation and ownership of the risks by key personnel;
- Risk audit interviews – conducted by experienced managers and/or external specialist advisers, with all those involved in the programme;
- Risk workshops – including all members of the project team and wider staff and stakeholder partners.
The following areas of risk will be considered to assist the identification of a comprehensive register of risks specific to the programme.
- Patient risks – the risk that patients are adversely impacted (for example in terms of patient experience, safety and outcomes of care) during transition and implementation of the proposed Agreed service model;
- Business risks – the risk that the Trust cannot meet its business imperatives (e.g. quality, safety, performance standards);
- Reputational risks – the risk that there will be an undermining of patient and public /media perception of the Trust’s ability to fulfil its business requirements – for example, adverse publicity concerning an operational problem;
- Service risks – the risk that the new service model and estate solution is not fit for purpose;
- Design risks – the risk that design cannot deliver the services to the required quality standards;
- Planning risks – the risk that the implementation fails to adhere to the terms of the planning permission or that detailed planning cannot be obtained; or, if obtained, can only be implemented at costs greater than in the original budget;
- Build risks – the risk that the construction of physical assets is not completed on time, to budget and to the required specification of quality and design;
- Contractor risks – the risk(s) that external contractors may for example experience financial difficulties, may not effectively manage sub-contractors, or that the interface between different contractors on the CRH site is not effectively managed;
- Project intelligence risk – the risk that the quality of initial intelligence (for example, preliminary site investigation) will impact on the likelihood of unforeseen problems occurring;
- Decant risks – the risk arising in accommodation projects relating to the need to decant staff and patients from one site to another;
- Environmental risks – the risk that the project has a major impact on its adjacent areas;
- Procurement risks – the risk that procurement fails to identify a supply chain partner and / or secure appropriate contractual arrangements;
- Operational risks – the risk that operating costs vary from budget and that performance standards slip or that a service cannot be provided;
- Demand risks – the risk that the demand for a service does not match the levels planned, projected or assumed;
- Volume risks – the risk that actual usage of the service varies from the levels forecast;
- Maintenance risks – the risk that the costs of keeping the assets in good condition vary from Budget;
- Technology risks – the risk that changes in technology result in services being provided using sub-optimal technical solutions;
- Funding risks – the risk that the availability of funding leads to delays and reductions in scope as a result of reduced monies;
- Residual value risks – the risk relating to the uncertainty of the values of physical assets at the end of the contract period;
- Economic risks – the risk that project outcomes are sensitive to economic influences – for example, where actual inflation differs from assumed inflation rates;
- Financial and affordability risks – the risk that the project costs of transition and implementation exceed the budget plan for this. Also the risk that implementation of the proposed future model does not generate the anticipated level of efficiency savings;
- Legislative risks – the risk that legislative change increases costs;
- Policy risk – the risk of changes in policy direction leading to unforeseen change.
- Adjacency risk – the risk that services in adjacent areas will alter or be reconfigured changing the demands upon CHFT services (may be positive or negative).
- Lack of clinical staff engagement – the risk that staff currently providing the services do not engage and participate in the project and therefore key advice and input regarding the design and implementation of the service changes is not secured.
The key risks identified will be entered into a risk register. Each risk will be scored 1-5 in terms of its likelihood and the severity of its consequences this will be the inherent risk (i.e. risk exposure with no mitigation). Once a risk has been scored, the controls and mitigation actions available will be analysed and a mitigation owner identified. The actions required to mitigate the risk will be identified in the risk register, with named responsible officers and information on progress. A residual score will also be included, showing how progress on mitigation has affected the level of risk.
On a monthly basis the Programme Board will review the risk register. All programme risks with a risk score of 15 or more (calculated by multiplying likelihood by consequence) will be escalated on a monthly basis to the Trust’s Audit and Risk Committee and the Trust Board. The role of the Trust Board will be to assure itself that all risks are accurately identified and mitigated adequately.
11.3.2 Current Risks
Progress of the proposed reconfiguration of hospital services is currently included on the Trust’s Board Assurance Framework as a high level risk. The risk is related to not being able to progress service reconfiguration and as a consequence that there are delays in addressing important quality, safety and sustainability issues such as:
- Patient safety risks associated with dual site services and not having critical clinical service adjacencies;
- Compliance with emergency medicine standards;
- Compliance with paediatric standards;
- Compliance with critical care standards;
- Difficulties in recruiting and retaining a medical workforce (continued and increased reliance on middle grades and locums);
- Increased gaps in middle grade doctor rotas;
- Delays in the Trust’s financial recovery plan and continued reliance for a longer period on financial support from the Department of Health and Social Care;
- Inability to contribute to improvement and achievement of the local and West Yorkshire system affordability;
- Inability to sustain the condition and reliability of building and engineering services infrastructure at HRI and that retrospective building regulations will be introduced;
- Risk of negative impact on the Trust’s reputation.
The Trust Board will continue to regularly review these risks and the interim necessary actions that are required to mitigate these risks as far as it is possible to do so.
11.4 Benefits Realisation
The ultimate responsibility for the delivery of the programme benefits rests with the SRO for the project. The Programme Board will agree a benefits realisation strategy setting out arrangements for the identification of potential benefits, their planning, modelling and tracking. It will also include a framework that assigns responsibilities for the actual realisation of benefits throughout the key phases of the programme.
A Cost Benefit Analysis (CBA) methodology will be used during the programme and be based on best practice described in the Treasury’s Green Book. The CBA will estimate the overall public value created by the programme including economic benefits to individuals and society; and wider social welfare/wellbeing benefits. It will also determine the financial impacts for the Trust and estimate the financial impacts across partner agencies affected. The Programme Board will receive regular update and review of the CBA.
All benefits will be entered into a benefits realisation register. For each benefit this will include the following information:
- Service feature (what aspect of the programme will give rise to the benefit – to facilitate monitoring);
- Potential dis-benefits;
- Activities required (to secure benefit);
- Responsible officer;
- Performance measure;
- Target improvement (expected level of change);
- Full-year value;
- Timescale for realisation of the benefit.
On a monthly basis the Programme Board will review the benefits register. Any expected benefits that are ‘off-track’ (i.e. not delivering as planned) will be escalated on a monthly basis to the Trust Board. The role of the Trust Board will be to assure itself that all benefits are accurately identified and their realisation is being effectively managed. Some of the key programme benefits that will be included on the register include:
- Improving the quality of patient experience through more streamlined, efficient patient pathways as a result of the reconfiguration of services.
- Realising patient outcome benefits from co-location of acute services and consolidation of paediatrics with complex obstetrics through a more streamlined approach for providing senior medical oversight.
- Supporting the development of urgent care centres which will be equipped to care for patients with minor injuries and / or illnesses in a more timely, efficient way.
- Enabling the Trust to meet the Royal College of Emergency Medicine standards on senior medical workforce cover.
- Enabling the Trust to meet Royal College standards for Children and Young People in Emergency Care settings.
- Reducing the reliance on locum and temporary staff to cover vacancies and workforce pressures as a result of running two district general hospitals.
- Making the Trust a more attractive place to work thus improving the recruitment and retention of staff.
- Improving clinical rota resilience: rota frequency will reduce immediately with the consolidation of some services thereby reducing the workload strain on staff and improving the resilience of services.
- Enabling sub-specialisation of clinical services: the critical mass achieved through consolidating of unplanned patients and workforce onto one site will allow greater opportunities for subspecialisation of the workforce improving the attractiveness of employment at the Trust and enhanced clinical services for patients. Relevant services include paediatrics and trauma subspecialisation in emergency department, and acute medicine.
- Improving skill mix / role improvements: Advanced/Extended scope Practitioner role will be further refined and deployed in the Trust to reduce reliance on the middle-grade doctor workforce across many specialties including ED, acute medicine, and paediatrics.
- Improving junior doctor training, oversight and supervision: junior doctor training and supervision is anticipated to improve for all clinical services being consolidated on to one site given the increased throughput of activity, and the increased non-locum consultant presence on site. This will also apply to other clinicians in training.
- Reducing long term sickness absence: the benefits above will allow for more effective service planning. This, together with other measures to support staff returning from absence, will help to reduce stress for staff and reduce the Trust’s long term sickness absence challenge.
- Improving the patient care and staff working environment. The capital investment at HRI will enable adaptation of existing buildings and address the most critical maintenance requirements to enable the continued use of some of the existing site.
- Elimination of the Trust’s deficit and enabling wider system affordability and resilience.
12 Stakeholder And Public Engagement
The Trust will continue to fully engage and involve local people, key stakeholders and the Joint Health Scrutiny Committee in the next steps to deliver the proposed future model for hospital services across Calderdale and Greater Huddersfield. This will be an ongoing process throughout the decision-making timeline described in section 2.
The aim of the engagement activity is to ensure the local NHS:
- Continues to engage and involve local people, and key stakeholders as more detailed plans are developed to deliver the proposed future model for hospital services across Calderdale and Greater Huddersfield;
- Continues to understand the changing demographics of our local communities and how this relates to service use, access and patient experience;
- Can demonstrate that any potential differential impact on any protected groups is captured and considered.
The local NHS will continue to work closely with the Calderdale and Kirklees Joint Health Scrutiny Committee. Informal workshops and meetings took place in July and August 2018 and the proposals were discussed at the formal public meeting of the Joint Committee that took place on 7th September 2018. Since then further informal meetings with the Joint Committee Chairs were held on 1st October 2018, 5th November 2018 and 22nd January 2019. A formal public meeting of the Joint Committee was held on the 15th February 2019 to further discuss the proposals and this included the plans described in this section for further
stakeholder engagement.
There will continue to be on-going engagement with Calderdale and Kirklees Councils.
The revised hospital model is an evolution of the proposals informed by previous engagement and the significant public consultation undertaken in 2016.
There are a number of areas where the proposed model is therefore unchanged from that which was previously the subject of public consultation (this includes: urgent care; maternity and midwifery services; paediatrics; planned surgery; acute inpatient medical care; critical care; acute and complex surgery, and; outpatient services).
Where changes have been made to the proposed future hospital service model this has sought to respond to the views of stakeholders and to the recommendations of the IRP. The key changes are: the continued provision of 24/7 consultant-led A&E services at both sites; the provision of physician-led inpatient care at HRI, and; a commitment to maintain the number of hospital beds broadly as they are now whilst services are developed in the community.
The approach to engagement will be inclusive and will include a range of opportunities for the public and stakeholder groups to provide their input and insight.
The areas that are identified as requiring further involvement from local people are:
- Development of hospital services
- The design and development of buildings and estates with specific focus on;
- The development of Calderdale Royal Hospital estate as a central emergency site (including co-design of the environment)
- Co-design of a dedicated paediatric centre at Calderdale Royal
- The refurbishment of Huddersfield Royal Infirmary including co-design of a children and young people friendly waiting area at A&E
- Travel, transport and parking for both hospital sites
- Use of digital technology
- Care at or closer to home
Further engagement will be based on the following principles:
- Ensuring we engage with the public, patients and carers early enough throughout this process;
- Being inclusive in our engagement activity and considering the needs of our local population;
- Ensuring that engagement is based on the right information and good communication so people feel fully informed;
- Ensuring that we are transparent in our dealings with the public and discuss things openly and honestly;
- Providing a platform for people to influence our thinking and challenge our decisions;
- Ensuring that any engagement activity is proportionate to the issue and that we provide feedback to those who have been involved in that activity;
- Ensuring we are clear about our plans and what the public can and can’t influence and why;
- Making sure we engage with the right target audience and consider equality and the impact on diverse groups;
- Demonstrating that we have listened to people’s views in all of our plans;
- Providing feedback on our website.
The involvement of groups protected under the Equality Act will be targeted to ensure that the needs of these groups are understood, and due regard is had to advancing equality in developing, making decisions about, and delivering the proposed changes to services in Huddersfield and Calderdale. The protected groups that will be targeted are:
- Age – specifically children and young people, older people, and frail elderly;
- Gender;
- Disability;
- Ethnicity representative of the demographics of Greater Huddersfield and Calderdale;
- Religion and religious belief;
- Sexual orientation;
- Transgender;
- Pregnancy and maternity;
- Carers.
All engagement activity will be informed by local data to assess the representativeness of the views gathered during the engagement process. An Equality Impact Assessment will be
prepared.
It is planned that the engagement activity required to deliver the next stages of development will be co-created at an initial stakeholder event during the Spring 2019. This event will be used to support the design of specific involvement activities and describe the communication material required to support the approach to ensure that local people remain informed and/or involved in the next stage of development for hospital services. The engagement will therefore take place in two stages:
Stage 1 (Spring 2019) – Stakeholder involvement in developing the action plan for engagement and associated communication material.
Stage 2 (Following the stakeholder event and then ongoing throughout the decision making process) – Delivering the action plan to involve a wider audience of local people.
The Trust and the CCGs will engage, involve and respond to the Calderdale and Kirklees Joint Health Scrutiny Committee in progressing these developments.
13. Letters Of Support
Letters of support for the SOC have been provided by:
- Calderdale CCG - Matt Walsh
- Greater Huddersfield CCG - Carol McKenna
- West Yorkshire & Harrogate Health and Care Partnership - Rob Webster
If you'd like to read these letters of support, please email us, ask.reconfiguration@cht.nhs.uk, and we'll send you a copy.
ANNEX A: Care Closer to Home – Additional Information
1. Background
In both Calderdale and Kirklees, integrated community and primary care services are being developed to meet the different levels of need of the local populations. Community based services will be led by multidisciplinary teams of health and care professionals, working together to meet the needs of people who have short-term health needs, individuals with long term conditions and those requiring specialist care for severe or complex needs. These services will be delivered over populations of 30,000 to 50,000 people in a way that makes it easier for people to access care when closer to home, with a consistent and high quality experience for patients as they move between different parts of the integrated system.
This work builds on strong existing working relationships between the GPs, community services and both Kirklees and Calderdale local authorities. Calderdale CCG has worked with Calderdale Local Authority to produce a Single Plan for Calderdale within the overarching vision of ‘Calderdale Cares’. The system’s strategy is to deliver an integrated, locality based, health and care offer, driven by population based commissioning and primary care led. Building on the CCG’s existing approach to primary care development and Care Closer to Home approach the aim is to improve care and quality of services and move the provision of care from unplanned to planned care, and the location from hospital to community. Development and delivery of the plan is overseen by the Health and Wellbeing Board. Greater Huddersfield CCG and North Kirklees CCG have worked with Kirklees Local Authority to produce the Kirklees Health and wellbeing plan. The vision for the Kirklees health and social care system in 2020 is: “No matter where they live, people in Kirklees live their lives confidently and responsibly, in better health, for longer and experience less inequality.” This place based system of care will include social care, community services and Primary Care initially and develop to include mental health, voluntary and other services and support in the future.
2. Introduction
In September 2018, with support from the West Yorkshire and Harrogate Health and Care partnership, Calderdale and Greater Huddersfield CCGs commissioned a piece of work, the
aim of which was:
‘To be able to clearly quantify the impact of interventions in primary and community care on reducing demand in acute settings, by being more rigorous about: which interventions work; how we could standardise their application; and the utilisation of underpinning data driven modelling to give confidence in delivery.’
Subsequent to this, a report has been produced for the CCGs that describes in detail the plans for out of hospital services and what their potential impact on acute hospital services could be. The report provides important information to support the development and delivery of the Calderdale and Kirklees place based plans.
3. Summary
The report identifies:
- The baseline position, the likely impact of currently planned pathway-based changes and the risks to their successful implementation.
- A realistic ambition for the potential impact of the CCGs’ longer term place based plans in which many or most community services would be integrated, co-located and work closely with primary care and social care to deliver care in the community from hubs serving localities of 30-50,000 people.
- An operating model describing how care could be provided to deliver the longer term plans, utilising Population Health management to identify the potential capacity required – in terms of both staff and estate – to operate a community hub within each of the CCGs’ identified localities.
- The factors to consider as part of any implementation.
3.1 The Baseline Position
Calderdale and Greater Huddersfield CCGs serve a population of 469,000 people. This will grow to 478,000 by 2023 (0.4% per year). As this increase is concentrated in the over 50’s where most of care takes place, actual demographic activity growth will be ~1% per year resulting in an expected 5% increase in activity from demographic growth over 5 years. If nothing changes, in 5 years our system will require 43 more acute beds
The current model is very fragmented in its service provision. Many different teams offer different packages to the same patients, and multiple teams will offer similar forms of care intervention but exclusively to patients with different conditions. As an example, there are over eight entry routes into community services across the two CCGs that are denoted “single points of access.”
The CCGs’ current plans are focussed on the populations placing greatest strain on the system (including the frail elderly, respiratory patients, and those awaiting transfers of care), and are designed to implement national best-practice in the delivery of care and design of pathways. Successful implementation of the CCGs’ currently planned pathway-based changes, could reduce non-elective bed days by 10% over 5 years.
3.2. The Operating Model
As recognised in the CCGs’ place based plans, improving the health of the population and achieving the potential 30% reduction in non-elective bed days is not about running more, or a different set of initiatives. The most successful systems redesigned their out-of-hospital care with a broad integration of services and teams, including social care. This section summarises
- The model of care provided by this integrated approach;
- the method for delivering care from co-located teams operating out of community hubs and the capacity this might require in each locality
3.2.1 What the proposed integrated case system would involve
Integrated community and social care systems provide 13 best-practice interventions or types of service to their patients. These range from individual case management and co-ordination of care services, through the rapid availability of specialist and primary care services close to patients’ homes, to intermediate care facilities. As a whole, the 13 interventions target the three main approaches to reducing hospital usage: they aim to proactively care for population health and prevent admissions; they provide care in alternative locations as appropriate; and they support quick and effective transitions of care between settings, including out of the hospital.
These 13 types of service are then tailored to the specific needs of the local population. Highneed patients would receive more frequent intensive support. Patients with lower needs would receive timely access to appropriate care when needed alongside self-empowerment of care and education. To make this work, a needs-based stratification of the population is required to say both how many patients are in which need group and to identify exactly which patient needs which level of support. In this way, the right care is designed and provided for each patient. The report describes what this model might look like in terms of the care provided to a high-need, medium-need and low-need patient. This includes a description of their initial assessment by a multi-disciplinary team, the care package constructed using the 13 types of service, and what this means in terms of their average contact time with nurses, doctors and other health and care professionals.
3.2.2 How care would be delivered, and the capacity required to do it
Central to the success of the best systems is the co-location and integration of all out of hospital services based within and around community hubs. The community hubs would serve localities with populations of 30,000-50,000 people. Care provided by the hubs would be designed and organised by a central multi-disciplinary team, with a clear point of accountability for delivery of all out of hospital care in the locality. In Calderdale and Greater Huddersfield, this would mean that the existing programmes and level of care would still be provided, but teams with similar functions (for example, the various home visiting services provided by nurses or healthcare assistants) would be unified.
Remodelling care in this fashion often means that a different mix of skills is required in the workforce, but this does not necessarily imply the levels of growth in the number of doctors or specialist nurses that would be required if we simply grew our current model of care to meet future demand. The report sets out, for each locality, the average contact time for patients with different needs per year, and the estimated workforce requirements by role, as well as our likely requirements for community beds and estate. To deliver an integrated model of care across both CCGs by 2023 would require a total of: 2000 FTEs, of which 157 would be a new role of Care Navigator; 169 community beds; and about 13,000m2 of estate. The assumptions that drive this forecast can be adjusted within each locality, to reflect the packages of care designed for each population group by the local care providers and networks of GPs. The size of each locality will affect to some extent the services that can be provided economically within each hub. For example, all elements of pro-active and preventative care (MDT assessment, case management and care co-ordination) can be provided in hubs that serve 30,000 people, but the minimum efficient scale for an urgent care centre to operate is for populations of around 50,000.
The capacity and resource requirements described in the report focus on an efficient endstate, with services provided at scale. It may be that the CCGs decide to provide sub-scale services, for example to increase provision to populations in very rural areas: this would require additional resources for care delivery.
3.3. The factors that will enable the transformation
The CCGs have a good track record of piloting new services, then successfully rolling them out across the area. However, to run a complete transformation of their community services, additional focus and further work would be required on seven principal enabling factors.
- A. Change management for patients and staff. Re-organising community and social care will not be possible unless clinical staff and patients understand and believe in the benefits of change. Some GP networks are already engaging with the programme, but clear role modelling from committed clinicians will drive later engagement and success. Likewise, we would need to engage patients to understand how to get the most from our new model of care, empowering them to shape its development and ultimately take greater control of their own health.
- B. Organisational design. Locality based hubs will lie at the centre of an integrated primary, community, mental health and social care offer in each locality. While this will inevitably involve collaborative working across different professional groups, both the development and operation of these integrated services will need to proceed under a single accountable manager who is able to manage and coordinate the activity of contributing staff. Even if care is delivered through a partnership between different providers, having a single accountable person with the authority to decide how care will be provided is a common feature of successful systems.
- C. System-wide ownership and accountability. While a single manager should run the services in each locality, oversight is likely to be provided by a partnership board. This group should be able to hold the manager to account for progress and performance. Additionally, it should be a means for the manager to quickly access executive-level support when challenges arise.
- D. Funding. It will be important to identify funding to ensure there is sufficient capacity within the new model of care.
- E. Ensuring contractual incentives are aligned. We will need to work closely with our providers to ensure that the balance of incentives between acute provider, primary care networks, and community care providers are aligned with us around improved and more cost-effective patient care.
- F. Information sharing. Timely flow of clinical information between all relevant health professionals is a crucial enabler for our new model of care. In addition, we will need to track the performance of our new model in order to ensure that it is delivering intended benefits.
- G. Digital and analytics. The completion of the Yorkshire and Humber Local Health and Care Record Exemplar programme will provide a fantastic foundation. This will give all care providers appropriate access to care records, greatly facilitating the co-ordination of patients’ care. However, this is only the tip of the iceberg in terms of the potential benefits it could help us to deliver. We will need to develop our capability to provide detailed analytics and reporting as part of future improvements to care – focused on those cases that can have the biggest impact.
The diagram illustrates the new or expanding schemes across Calderdale and Greater Huddersfield that will address non-elective hospital usage.