Foreword
In December 2018 the Department of Health and Social Care announced that £196.5m of public capital funding had been allocated for investment at Huddersfield Royal Infirmary and Calderdale Royal Hospital. In 2019 CHFT published a Strategic Outline Case that described the future service model and the benefits investment in hospital buildings will enable by modernising care pathways, improving clinical adjacencies, and ensuring high quality, and sustainable health care facilities into the future.
This report is the next stage of a continuous process of public and colleague involvement to ensure we focus on what’s important.
In developing this report patients, members of the public, stakeholders and colleagues have shared their views on what matters to them. They have described their aspirations for modern health services, delivered in buildings that offer a healing and therapeutic environment that is welcoming, calm and provides a light environment with external views; is accessible and inclusive supporting diverse patient needs; that ensures privacy and dignity, and; enables social interaction.
Their involvement has informed the design principles described in this document. A key principle is that both hospitals will be “digital by design”, ensuring modern working practices through better use of technology. Digital will be at the heart of our future hospital operations ensuring efficient patient flow, improved patient and colleague experience, and best use of resources.
The design principles set out in this document will underpin how we move forward to develop the detailed design plans for investment in both hospitals and ensure we can continue to deliver outstanding compassionate care to the communities we serve for future generations. We will continue to involve and work closely with patients, members of the public and colleagues to ensure that:
- We put the patient first
- We ‘go see’
- We work together to get results
- We do the must-do’s
Owen Williams
Chief Executive
Peter Wilkinson
Chair of Transformation Programme Board and Non-Executive Director
1 Introduction
Calderdale and Huddersfield NHS Foundation Trust (CHFT) is an integrated Trust that provides acute and community health services. Hospital services are provided at Calderdale Royal Hospital (CRH) and at Huddersfield Royal Infirmary (HRI). The distance between the two hospitals is just over five miles. The Trust also provides community services in the Calderdale area.
This Design Brief has been prepared to inform and support the development of future design and construction schemes across the CHFT estates. The principles identified within this document represent the design parameters that the Trust seeks to be embodied within any future refurbishment, extension or new build project, reflecting its core objective of creating state-of-the-art facilities that will support delivery of 21st century healthcare services for the local community and beyond and enhance the immediate surroundings of its estates. The document seeks to:
- Describe the overarching principles that the Trust is seeking to incorporate, not only into the design of new accommodation but also the adaptation / improvement of existing estate;
- Identify key clinical and non-clinical adjacencies and establish key patient flows and connectivity;
- Capture the physical requirements and aspirations for relevant clinical and non-clinical services; and
- Describe the operational processes affecting clinical specialities.
It should be recognised that the principles identified within this document represent the Trust’s design aspirations: it is recognised that these may not, and indeed in all likelihood will not be achieved in all cases. However, they articulate an appropriate challenge to any future design or construction team responsible for the delivery of accommodation that best reflects the Trust’s values, ideals and ethos.
1.1 Background to the document
This Design Brief was developed by the Trust with support from Mott MacDonald and IBI Group during the period September 2019 to January 2020. It is the outcome of extensive discussions with a cross-section of colleagues from the Emergency Department, Medical and Surgical Inpatient Wards, Surgery and Theatres, Imaging and Diagnostics, Education & Training, Facilities and Support Services, and Health Informatics.
It also specifically draws upon feedback from public engagement sessions with local healthcare stakeholders, voluntary organisations and members of the public with a strong interest in the way healthcare services are delivered in the region, and which were attended by more than 150 colleagues, stakeholders and members of the public. These sessions helped to define an overarching set of principles and themes that should be used as a barometer during the development of any design solution.
In addition, the Design Brief builds upon significant public, stakeholder and clinical engagement undertaken by the Trust since 2012. To date, discussions have involved engagement with primary and secondary care senior clinicians; external clinical review via NHSE; system meetings with regional leads for NHSI, NHSE and the Integrated Care System; Health & Wellbeing Boards; Joint Health Scrutiny and Local Medical Committees (LMCs). The Trust will be continuing to engage and involve local people, voluntary organisations and key stakeholders in the next steps to deliver the proposed future model for hospital services across Calderdale and Huddersfield.
1.2 Structure of this Brief
The structure of this document has been purposefully crafted in order to lead the reader into a design process. The aim is to be clear regarding the aspirations of the Trust whilst providing flexibility for designers and engineers to innovate, challenge and deliver excellent solutions.
The Introduction sets the scene and objectives of the Trust whilst the Approach to Design articulates how a design is to be executed and evaluated. It seeks to define a process which follows clinical pathways as a design development strategy (rather than individual clinical departments) and highlights strategic key adjacencies which are to be achieved / maintained.
The Design Vision sets the aspirational tone of the Trust. The Vision provides a clear articulation of outcomes which we expect a design team to resolve and exceed. It is purposefully “outcome” driven and provides the designer with parameters that are to be achieved in a coordinated form. Furthermore, design exemplars allow the Trust to ‘show’ what they’ve seen previously and liked.
Clinical Design Principles are specific to the project in hand and utilise information gathered from Trust clinical workflows. This information is often distilled from the notes of the engagement sessions. However, the information is included to help inform the design team.
The Functionality section allows the Trust to set the necessary functionality tone for the design, principally how the hospital is to operate, the flexibility it needs to contain, specifics around access, security, wayfinding. Whilst the Character and Innovation section sets a style tone for the design.
Finally, the Design and Construction Standards highlight the importance of alignment to published technical and national best practice, reaching beyond simple compliance with HBN’s and HTM’s.
1.3 Strategic Context
People in Calderdale and Huddersfield are living longer. However, a greater number are likely to have multiple long-term conditions thereby increasing demand on the health and social care system.
Nationally growing shortages of a qualified clinical personnel has increased use of agency and other temporary workers to fill vacancies, and in turn, this has increased NHS expenditure and made services less stable. This national workforce pressure is exacerbated by the current dual-site configuration of most CHFT services, making it difficult to recruit and retain the necessary permanent human resources and leading to a reliance on temporary and agency personnel (with associated higher costs) to sustain service delivery.
CHFT has consistently delivered a high level of performance against national access targets and was given an overall rating of “Good” by the Care Quality Commission (CQC) in 2018 (this combined rating included “Requires Improvement” for the Use of Resources). Over the last two years across the combined and ranked metrics of Referral to Treatment Times (RTT), Emergency Care Standard (ECS) and Cancer waiting time less than 62 Days, CHFT has consistently been one of the best performing Trusts in England.
CHFT is one of the most digitally advanced Trusts in the country and this will continue to be key to enabling delivery of high standards of performance.
1.4 Critical Success Factors
The Trust has identified the following critical success factors / overarching design objectives for its new developments, against which developing design solutions will be benchmarked at successive project gateways;
- "A Good Neighbour": developments must respond creatively to the constraints and opportunities presented by their sites and contribute positively to their local and wider environments;
- High Quality: developments must be inspiring, humane and attractive, providing high quality, functional and enduring environments reflecting a strong positive image of the NHS and the Trust and supportive of the delivery of excellent clinical services for the people of Calderdale and Huddersfield;
- Digital by Design: the design of buildings must enable and support the Trust’s ambition to ensure the optimal use of digital technology and associated new ways of working in the delivery of healthcare;
- Efficiency: developments must make a positive contribution to the efficiency of the clinical services delivered by optimising departmental locations, taking account of desirable clinical adjacencies and ensuring efficient colleague, patient, visitor and Facility Management (FM) flows;
- Accessibility: developments will need to incorporate prominent and conveniently located main and departmental entrances and be organised around an intuitive and readily comprehensible circulation arrangement that aids wayfinding and orientation;
- Flexibility: developments must be capable of accommodating a wide range of changes throughout their lifespans (e.g. the reconfiguration of clinical services, the introduction of new technologies and adjustments to spatial requirements) with minimum disruption to ongoing service delivery;
- A Healing Environment: developments will be required to provide a therapeutic environment for patients, their families / carers and an exceptional working environment for colleagues, promote wellbeing, and avoid appearing excessively clinical or institutional.
- Sustainability: developments should incorporate optimised design solutions aimed at minimising energy consumption and carbon emissions during construction and operation whilst ensuring compliance with the NHS Long Term Plan, as well as the relevant clinical, financial and environmental legislations and standards;
- Innovation: developments are to be planned with appropriate flexibility to ensure “future readiness” in accommodating innovative developments in operation and equipment;
- Safety and Security: developments must provide a safe and secure environment for all patients, their families / carers and colleagues, ensuring that the safety, privacy and dignity of all individual users is maintained, and that the Trust’s Infection Control Strategy is fully implemented as well as ensuring ease of access for maintenance of kit and equipment;
- Natural Light and Ventilation: developments will be required to maximise the availability of natural light and ventilation where clinically or operationally appropriate, minimise glare and excessive solar gain and provide attractive views of visually stimulating areas.

Source: Dana Faber Cancer Institute.

Source: Working natural light in healthcare: spaceforhealth.com.au
The Trust wishes to thank all the organisations and companies that gave permission for their images to be used in this document.
2 Approach to Design
The Trust is keen to achieve high-quality design solutions, which provide caring and working environments for patients and colleagues that support delivery of high-quality clinical care.
In order to benchmark the development of such solutions, designs will be evaluated throughout their development using the “Achieving Excellence Design Evaluation Toolkit” (AEDET Evolution), published by NHS Estates.
2.1 Trust Governance of Design
The CHFT Transformation Programme Board (a formal sub-committee of the Trust Board) is responsible for ensuring that the principles of good hospital design are incorporated at every stage of the development and to provide assurance to the Trust Board regarding this.
2.2 BREEAM
In order to assess their impact on the environment, the sustainability measures associated with design solutions will be assessed and scored using the Building Research Establishment’s Environmental Assessment Method (BREEAM) Healthcare. New developments will be expected to achieve an “Excellent” rating as mandated by Department of Health and Social Care (DHSC) guidance.
2.3 Clinical Pathways
The Trust adopts the approach of considering the clinical pathway, mapping the flow of activity and patients through the hospital, rather than individual departments. In adopting this approach, the Trust are keen to ensure that all interdependent relationships are maximised in order to achieve optimum efficiency.
As such, future design exercises are required to look at the interdependencies and relationships between all aspects of healthcare delivery.
2.4 Service Adjacencies
Key functional movement requirements include:
- Emergency Departments must have direct external ambulance entrances and an external access point for ambulant users;
- Emergency routes to and from Emergency Departments (ED) must be as direct as possible and cross flows with outpatients and visitors must be avoided;
- Direct internal access is required to permit the efficient movement of patients between Emergency Departments, Radiology, Operating Theatres and Critical Care Unit;
- Facilities Management (FM) entrances should be provided away from main public entrances with vehicular waiting areas and materials storage areas concealed from direct public view. Central FM services should be provided away from patient, colleagues and visitor areas. FM services within clinical departments should be zoned to minimise cross flows with patients and visitors; and
- Access to Mortuaries for the transportation of deceased patients must be discrete and not pass through publicly accessible areas.
A more detailed analysis of clinical adjacencies is included in Section 4.
2.5 Design Evaluation
Design proposals will be carefully scrutinised to ensure that;
- New developments and their surroundings promote civic pride;
- Developments give a strong first impression;
- High quality materials and construction are used throughout;
- The optimal patient and public experience is taken into account;
- The views of patients and colleagues are considered;
- Developments integrate positively with the surrounding urban / suburban fabric;
- Facilities are fit for purpose;
- Developments incorporate modern technology and support the Trust’s IT equipment;
- Developments enhance the sustainability of the Trust; and
- Developments are flexible and innovative in form and construction.
In order to achieve these objectives, this document sets out a series of Design Principles which broadly align with the “Functionality” and “Impact” components of Health Building Note (HBN) 00-01 General Design Guidance for Healthcare Buildings – i.e. those considered most pertinent in forming an early stage Design Brief. However, it is anticipated that this document will grow with the subsequent stage of Business Case development, capturing Trust policies as they relate to design and developing into a robust and comprehensive Design Brief to be used by Design Teams to inform their approach.
3 Design Vision
The Trust’s Vision is to develop excellent healthcare facilities on attractive and accessible sites that form an integral part of the Calderdale and Huddersfield area.
These facilities shall:
- Function well;
- Facilitate patient-centred care;
- Be delivered within attractive buildings and surroundings;
- Support delivery of leading-edge clinical services;
- Provide therapeutic environments to aid recovery;
- Offer appropriate flexibility;
- Support diagnosis and treatment, increasingly on an outpatient or day case basis;
- Enable the integration of services with those outside hospital;
- Support a highly skilled, professional workforce;
- Be operationally and environmentally sustainable; and
- Project a strong positive image of the NHS and the Trust.
Design solutions must capture the aspirations of as wide an audience as possible and provide humane, attractive, flexible and sustainable facilities that are distinctive and welcoming, whilst cost effective in capital and operational terms.
Designs should not only comply with defined spatial requirements but also address the psychological perception of space, including orientation, mobility, confidence, assurance, privacy and socialisation, within environments that offer sensory and visual stimulation to patients, their families / carers, and colleagues, and demonstrate variety and visual identity.
The locations and layouts of new facilities should embody efficient planning solutions to ensure the achievement of both quality and economy of cost and should incorporate appropriately convenient and functional links to associated existing accommodation.
3.1 A Healing Environment
The overall design philosophy adopted should be one that supports and accelerates the physical and mental healing processes in creating truly therapeutic environments.
Evidence Based Research, Biophilic Design and other innovative design approaches should be harnessed to deliver such optimal patient healing environments. The design ethos should also address key drivers such as: privacy, dignity, choice and control, social support and communication that can all impact on patient recovery and wellbeing.
3.2 Digital
CHFT recognises the transforming power that digital has to improve access to services and support people in managing their health, to ensure health and care professionals can access patient records wherever they are, and to provide decision support and artificial intelligence to apply best practice and eliminate unwarranted variation in care and outcomes.
CHFT is recognised as one of the most digitally advanced Trusts in the UK and has the ambition to develop beyond clinical systems to ensure that all colleagues and the processes used by them are digitally enabled.
In the next 5 – 10 years CHFT expects the existing model of care to look markedly different and will be offering a ‘digital first’ option for colleagues, patients and the public.
It is therefore essential that the building design, project management and construction of the developments at CRH and HRI are based on
- full understanding of the Trust’s digital ambition and the impact digital technology will have on the future healthcare operating model for colleagues and the public; and
- the optimal use of technology in the design, project management and construction phases of the capital developments to achieve benefits and savings related for example to time, safety, cost, and environmental sustainability.
CHFT aim is to see the use of digital technology as an enabler to positive clinical outcomes and fundamental to the developed clinical workflow. Constructive digital disruption to the healthcare planning process may be one way in which the Trust can better achieve its aspirations in this regard.
Digital as an enabler to better clinical outcomes and to drive improved safety, quality and efficiency is a critical success factor for the capital investment project at CRH and HRI.
3.3 Biophilia in Healthcare Design
The innate human need for contact with nature underpins the principle of biophilic design, which seeks to create ‘habitats’ for people within the modern built environment. The proven positive impacts to human health include improved cognitive function, reduced stress, improved mood, restored attention, and enhanced productivity.
The Trust recognises that as their Transformation Programme moves from the planning stage, through design to implementation, each intervention, be it a refresh, refurbishment, reconfiguration or new build, will generate opportunities to apply at least some of the principles of biophilic design. Embedding these principles at the outset will have a proactive and positive influence, not only on the wellbeing of colleagues and users of the facilities, but also improved clinical outcomes for patients. There is a body of academic research on biophilia in healthcare environments spanning nearly 40 years identifying positive outcomes ranging from reduced length of stay in hospital to reduced prescription of pain-related medication.
Through formal consultation and, more recently workshops with the public and colleagues, the Trust has received a wealth of feedback reinforcing the importance that users place on biophilic design in the type of healthcare facilities they wish to experience in the future.
3.3.1 Nature in the Space
External views of nature, and access to natural daylight should be provided to all patient and visitor areas as well as rest facilities for colleagues. Physical access to the outdoors should be provided where possible.
Internally, the inclusion of well thought out planting is an obvious and effective way to include natural elements within the environment. The presence of water in the form of an indoor water feature is a beneficial, though technically and operationally troublesome, addition to a space. However, there are many other ways to create a sensory connection to nature. The sounds, tactile experiences and patterns of nature can also contribute to the biophilic context and create a less clinical environment.
Natural daylight is essential to human wellbeing. In areas where access to natural daylight is not possible, electrical lighting could be designed to support physiological functions; although this may not be universally appropriate. Lighting patterns that vary across the day, mimicking circadian rhythms and promoting the biological effects of light on humans (melanopic lux) during daylight hours, can help to regulate alertness, digestion and sleep. Conversely, exposure to light at night can be particularly harmful to physiological rhythms, especially so in the hospital environment, which continues to operate as a workplace therefore night-time lighting should be minimised.
Variability is a key feature of the natural environment. Sounds are non-rhythmic and vary depending on the weather and location. Sensory stimuli such as the sound of running water or feel of a breeze are often absent from internal spaces, and this can be a stress factor. Where direct access to this is not possible, pink noise (natural sounds such as bird song, water, and wind) can be generated and used to provide analogues to nature in artificial environments. Introducing non-rhythmic sensory stimuli in this manner has been shown to reduce stress hormones and improve cognitive performance.
Where it is not possible to include natural elements, consideration should be given to analogues of nature that may be used in their place. For example, artificial planting is better than no planting at all as the human brain responds to biomorphic patterns, even those in non-living materials.

Source: nacarchitecture.com/images/lab/naturescure02.jpg.
3.3.2 Nature of the Space
Biophilic principles equate the arrangement of spaces to natural environments and seek to classify human psychological needs. Two particularly well evidenced biophilic principles are ‘prospect’ and ‘refuge’. In combination, the two conditions have a notable health response.
Prospect is a view over a distance, usually from a high position. It allows people to see themselves in context and promotes a sense of awareness and comfort. In the context of healthcare facilities, this could be safely incorporated using balconies and staircase landings with transparent barriers.
Refuge can be equated with the human need for shelter. This is the need for a small, protected area which allows audio and visual privacy. This can be achieved more readily in the context of healthcare facilities by incorporating booths, nooks or window seats in larger spaces. External landscaped areas might include gazebo-type structures, or a canopy of planting.
Not all of the principles of biophilia are as well evidenced as those described above and, in the context of a healthcare environment, the Trust has no appetite to promote ‘mystery’ and ‘risk’ within their overall Estate.

Source: https://www.payette.com/wp-content/uploads/archive/blog/2015/July/07-17-15_Biophilia/Diagram2.jpg.

Source: https://www.terramai.com/blog/wp-content/uploads/2018/06/randall-childrens-hospital-biophilic-hallway.jpg.
3.4 Sustainability
Healthcare facilities are some of the top energy consumers in the built environment. Driving down energy consumption can be challenging as they are heavily dependent on the building services required both for day to day operation like heating, ventilation and air conditioning, and for specialist systems like clinical gas distribution. Infection control drives the selection of many materials and technologies such as the use of radiant panels above ceilings rather than conventional radiators which can attract dirt, and the supply of fresh air to operating theatres and critical care units.
Heightened environmental awareness, public concerns about sustainable development, stringent environmental protection laws and the realities of climate change are altering the way healthcare providers operate. Several local authorities, including both Kirklees and Calderdale Councils in 2019, have announced climate emergencies and are looking at ways in which they can effect a change.
In addition, there is a growing awareness of the therapeutic benefits of good hospital design that can positively influence clinical outcomes, patient satisfaction and the performance of the workforce. Governments around the world impose strict sustainability requirements on healthcare buildings, but many providers elect to exceed regulatory requirements, aware that, through the integration of environmentally sustainable operations, they can cut their energy costs while creating a culture of nurturing and commitment for the wellbeing of both patients and personnel.
The Trust are looking for new developments within their estate to represent good practice and make a tangible step change in terms of both energy consumption and carbon footprint. Whilst the health, safety and wellbeing of patients and colleagues is primary, the Trust is required to demonstrate ways that their estate is improving and lessening its environmental impact.
The Trust are currently developing plans to reduce the emissions of greenhouse gases, waste arisings and local air pollution as part of requirements from NHS England.
3.5 Net Zero
In the UK we have legislated to be Net Zero on greenhouse gas emissions by 2050. Some local authorities and public bodies have stated that they will achieve this target sooner than this.
For the NHS, the aspiration of becoming a net zero emissions organisation presents challenges on a number of levels.
The NHS estate contributes approximately 20% of all emissions through the buildings, travel, transport and waste associated with their daily operation. Supply chain contributes the most significant element through the production and use of pharmaceuticals, food and catering, sanitation and emissions associated with the contracting out of healthcare services. The community also contribute to the emission profile, through travel to and from hospitals and practices but also in the use of pharmaceuticals at home (inhalers for example).
The Trust’s approach to this is to develop an estate which can contribute today to this target, but also adapt and flex to incorporate new and emerging technologies in the future. Ideally, buildings constructed today will be net zero over their full lifecycle. The use of fossil fuels as a primary source of energy will need to be carefully considered, and adoption of cleaner technology should be selected where appropriate. The Trust seeks to scale up the adoption of infrastructure and energy that support a net zero economy (e.g. electricity, hydrogen, biofuel).
The following form the core emission strategies of the Trust:
- All new buildings should be designed and built to be progressive in terms of energy demand (aiming for net zero carbon) and being highly energy efficient;
- Fossil fuel free primary energy sourcing;
- Refurbishment of existing buildings to make them much more energy efficient;
- Facilities to support the uptake and rollout of electric vehicles and supporting infrastructure
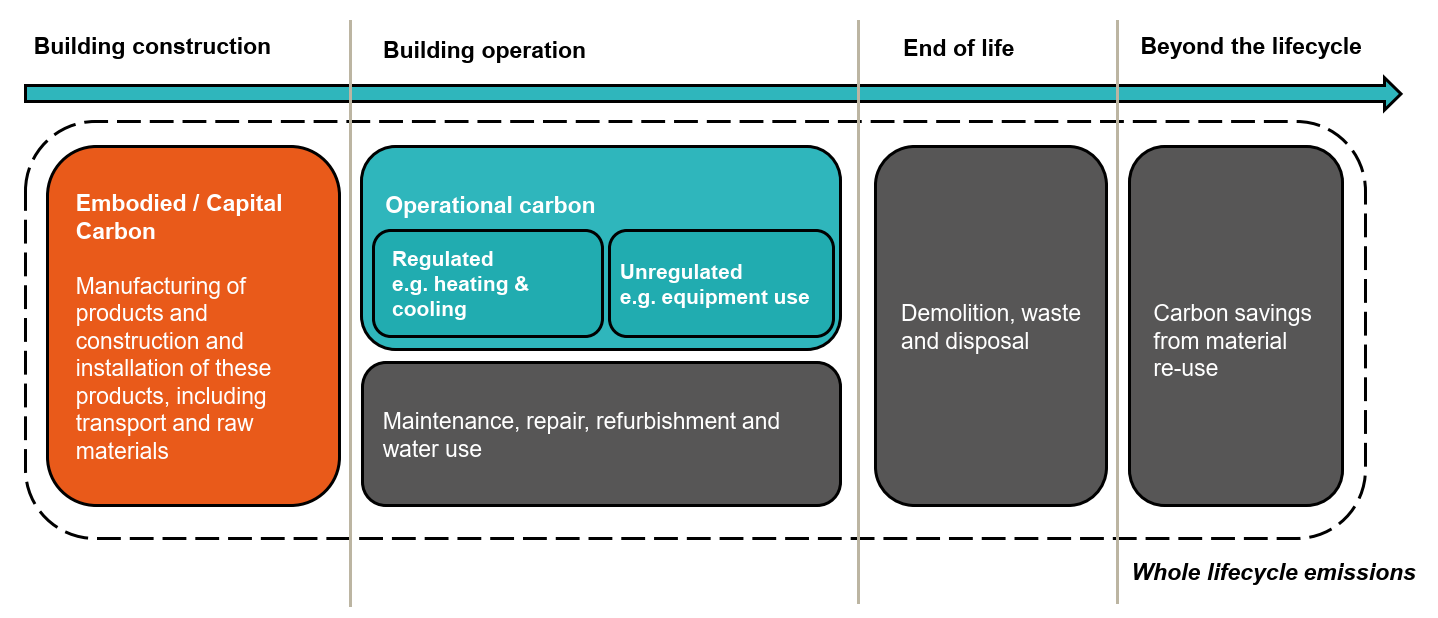
Figure 3.5 below demonstrates some of the characteristics to be considered when assessing the whole carbon lifecycle of a building.
Future projects will be expected to map this process in terms of carbon liability of the Trust.
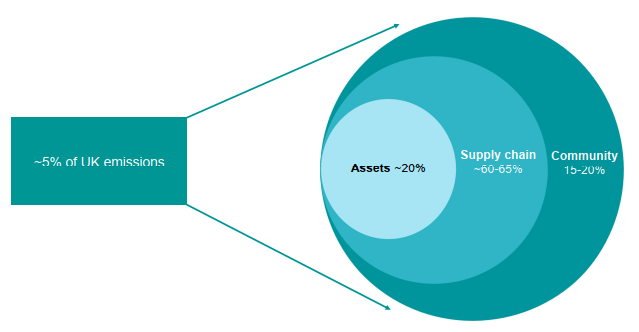
Source: NHSI values for Greenhouse Gas footprint (individual Trusts will vary).
3.6 Flexibility and Adaptability
Design solutions should be as adaptable as practicable in order to accommodate future change and diversification in treatments, technologies and management practice. They should be responsive to change and evolution and capable of accommodating change without compromising the overall design concept or service delivery. The strategy for adaptability should be achievable with limited disruption to services and at minimum cost.
3.7 Safety and Security
The safety and security of patients, visitors and colleagues is to be treated as a fundamental requirement of any design.
The maintenance of a safe and secure internal and external environment for patients, visitors and colleagues, together with maximum protection from / minimum exposure to potential crime, are essential. The Trust’s Emergency Departments deal with large numbers of people and consequently, a higher than average number of disturbances which require Police assistance.
3.8 Control of Infection
Infection control should be considered in all aspects of spatial design, construction, equipment specification, services strategy, commissioning, operational management and maintenance.
3.9 Privacy and Dignity
The Trust attaches great importance to the value of the individual – patients, their families / carers as well as Trust colleagues – and in developing any design, from masterplan through to individual room layouts, consideration must be given to the achievement of appropriate levels of privacy and dignity.
A prime objective should be to address privacy and dignity issues by segregating inpatient flows from ambulatory and visitor flows, including horizontal and vertical circulation. In particular, consideration should be given to the privacy of undressed or gowned patients.
3.10 Supportive Environments
Our immediate environment has a powerful impact on wellbeing, recovery and emotion. Designs should therefore address the particular needs of different patient groups, colleagues and visitors through a holistic approach to care and support.
Of particular importance, and a set of principles that have been echoed throughout the Trust’s consultation with stakeholders, is that designs should meet the needs of colleagues, patients and visitors with protected characteristics, such as age or gender reassignment, and be especially cognisant of those with disability or impairment (Equality Act 2010).
No-one should feel discriminated against when they use healthcare services and facilities, which may mean that they are treated differently in order to meet a particular need. Designs should apply a best practice approach to achieving supportive environments by removing the barriers to effective healthcare for those with physical or learning disabilities, autism and dementia. Section 5.8 provides an indicative structure that should be used to develop a supportive and therapeutic design strategy.
3.11 Design Examples
The following section includes a series of images from a variety of healthcare facilities and other public buildings which were used in either the Public or Colleague Involvement workshops and which prompted positive responses.
3.11.1 Ward Layouts
The following images seek to articulate some of the feedback from the public engagement sessions around ward composition and configuration.
Figure 3.6 was used as it demonstrated good ‘access to outdoors’ from the bedside via the large window, whilst also providing good connectivity to the nursing station through a large door and glazed panel.
Following on from this theme, Figure 3.7 demonstrated the provision of excellent natural light into a single bedroom.
Figure 3.8 identified an initial preferred configuration for multi bed bays. It was considered that for some patients, being in a multi bed bay would be beneficial from a social and medical perspective.


3.11.2 Wayfinding
A number of slides were presented during the public engagements in order to elicit feedback with regard to hospital wayfinding. Whilst all mentioned the use of digital as a source for improved wayfinding, the use of colour was highlighted.
Differentiating wayfinding for age groups (young, adolescent and adult) was considered positive whilst wayfinding which supported patients who were frail or had dementia would also be necessary.



3.11.3 Waiting Areas
There are multiple and sometimes conflicting demands from staff and patients who utilise the waiting areas. Some need the space to be calming, relaxing and meditative, whilst others need the space to offer an opportunity for mild levels of activity, the opportunity to move. A successful waiting area would meet the needs of both.
The use of natural light was preferred with artificial lighting used to supplement whilst adopting natural materials where possible. The timber slat ceiling in Figure 3.12 was identified as a good example of this.
It was recognised that seating in waiting areas needed to be robust, but this could be tuned to the specific department served. However, it was highlighted that often patients and visitors can spendsignificant amounts of time waiting for appointments, and therefore comfort is also a priority. It was suggested that Figure 3.14 appeared to strike a good balance.
Use of colour needs to be carefully considered with different options shown in Figures 3.13, 3.15 and 3.17.



3.11.4 Emergency Department (ED) Accommodation
The ED is a critical space within any hospital. Whilst public areas can present challenges in terms of security and comfort, it was agreed that strong design can mitigate some of these and enhance the overall impact of the space.
Again, colour was highlighted as a positive mood influencer. Too passive a theme and a space can be non-descript and boring, too active and the space can feel aggressive and agitated.
Space for young people and children to wait was considered helpful, although these would need to be observable from the regular waiting areas.
Patient privacy in cubicles was also discussed with the image in Figure appearing to offer high levels of patient privacy and dignity.



4 Clinical Design Principles
4.1 Key Design Requirements
Through engagement with both the public and clinical / non-clinical colleagues, the following specific design requirements were established. A number of these principles are further articulated and discussed later within this document:
- Where practicable, it is expected that horizontal and vertical flows for (i) Emergencies, (ii) Inpatients, (iii) Outpatients and visitors, (iv) highly clinical areas (e.g. Theatres) and (v) FM services will be separated, such that they do not cross, and there is clear demarcation between back-of-house and front-of-house flows;
- Adequate patient and visitor waiting areas should be provided in order to avoid obstructing circulation and / or impacting on the adequacy of fire escape routes;
- Designs should address accessibility, diversity and inclusion throughout the Trust’s estates;
- Reception areas and waiting areas should be welcoming with a range of seating and standing options available and, where possible, views of attractive external areas;
- The provision of natural lighting is deemed extremely important to users, who recognise the relationship between good natural light and improved recovery times;
- The selection of co-ordinated colours is important to users and colleagues with a preference for warmer, calming shades rather than “cool & clinical”;
- Wayfinding solutions should facilitate ease of movement around developments, including by those with hearing or visual impairment or for whom English is not their first language;
- Privacy and dignity are essential to patients, their families / carers, and colleagues from the moment they first step into a healthcare facility to the moment they leave or are discharged;
- The provision of carer’s overnight beds within some single bedrooms should be given significant consideration during the development of designs;
- With the increase in digital information and delivery of services, data security and privacy are a high priority;
- For inpatients, the hospital environment should promote social interaction with fellow patients, family, visitors and colleagues, whilst also providing spaces for reflection and ‘time-out’;
- Consideration given to gender neutral toilets; and
- It is anticipated that as part of any major development, the existing Main Entrance to Calderdale Royal Hospital will need to be supplemented with an additional point of entry for visitors.
This Design Brief focusses on, and presents the operational requirements of, the clinical workflows identified below. However, it is recognised that in seeking to satisfy the requirements and aspirations described, there will be impacts on other interfacing departments as requirements are better defined. Through this ongoing and iterative process, efficient overall design solutions are to be developed and harmonised.
- Emergency Department – Adult and Paediatric;
- Inpatient Wards – Medical and Surgical;
- Surgery and Theatres;
- Imaging and Diagnostics;
- Education and Training; and
- Facilities and Support
4.2 Emergency Department
4.2.1 Operational Functionality of ED
Key processes within an ED will include:
- Arrival (potentially via three entrances – majors, minors and paediatrics);
- Decontamination;
- Triage;
- Registration;
- Initial assessment;
- Assessment and treatment;
- Investigation;
- Discharge or admission.
4.2.1.1 Arrival - Site Access and Ambulance Bays
It is essential that the design of the external areas takes account of ambulance activity modelling to ensure sufficient ambulance bays are provided, enabling timely drop-off and turn-around of ambulances and minimising the risk of ambulances queuing. Patients arriving by ambulance should be admitted to the ED under a canopy that provides protection from the elements.
4.2.1.2 Arrival - Registration and Triage
- Generous Reception facilities, incorporating security screens, will be required to ensure patient confidentiality;
- The design should be arranged so that all adult patients (ambulant or arriving by ambulance) are conveniently brought to a single point where an initial assessment can be carried out to filter patients into Primary Care, Assessment Unit or ED;
- Triage and assessment areas must be adequately sized to ensure that patients are assigned to an appropriate pathway within their first hour of arrival;
- A key requirement is for any Paediatric ED to incorporate a dedicated entrance. A shared but appropriately visually screened Reception (e.g. children on one side and adults on the other) is however, acceptable;
- Elderly patients with dementia or delirium who do not mix well with the general ED population will be triaged, assessed and guided into a specialist Frailty Unit within 15 minutes.
4.2.1.3 Decontamination
If designated as a receiving centre for major trauma and chemical incidents, the ED will require a permanent Decontamination Unit rather than a tent type facility. An Isolation Room with Gowning Lobby will suffice. Spatial provision for a temporary facility will also be required to accommodate additional demand.
Such a facility will also serve as an emergency Infection Suite, eliminating the need to quickly, but temporarily close down other parts of the associated ED.
In the event of a Category A or chemical incident, specialised waste containers will need to be stored prior to removal and disposal.
4.2.1.4 Resuscitation
When determining the required number of Resuscitation Bays, the decision-making process should consider whether ‘spare’ (empty) Resuscitation Bays could be used to provide a ‘step-down’ High
Dependency Unit function, keeping potentially unstable patients who still require high levels of nursing care in the ED Resuscitation area rather than transferring them to Critical Care.
Dedicated Paediatric Resuscitation Bays are required, located close to the equivalent Adult facility as well as to the Ambulance Bay.
4.2.1.5 Assessment and Treatment
The design should seek to avoid pockets of disparate activity and instead, enable sub-Department boundaries to be flexed in response to demand.
The Trust’s ED teams are keen to move from couch-centric to chair-centric patient examination. This model provides better use of space. It is also the preferred arrangement for respiratory patients and for elderly patients who can decondition very quickly when laid down.
Chair-centric Treatment Cubicles present the opportunity to provide smaller spaces than couch-centric cubicles. However, it is expected that some patients may need to undress during assessment and diagnosis, therefore a couch may be needed for examination before the patient returns to a chair. The optimal size of chair-centric cubicles should be explored with colleagues during detailed design to ensure that the blend of furniture and equipment required can be accommodated.
Cubicles of each type should be of consistent size regardless of the initially planned function; i.e. Majors vs Minors.
It is expected that there will be a higher proportion of chairs vs couches in the Urgent Care Centre, compared to the ED. The balance needs to be established through further consultation with ED colleagues.
The use of “Procure22” type “repeatable” chair-centric and couch-centric cubicle layouts should be considered.
Those rooms allocated for patients with mental health issues should have good observation and be compliant with Royal College of Psychiatry recommendations. To ensure the availability of appropriate accommodation at all times, the possibility of making all cubicles suitable for mental health use through the introduction of manual pull-down shutters to conceal equipment (Nottingham University Hospital model) should be considered. All cubicles should be designed to be “ligature-light”.


4.2.1.6 Paediatrics
All paediatric patients (ambulant or arriving by ambulance) should arrive at a single point, separate from adult facilities, where an initial assessment will filter patients into Primary Care, Paediatric Assessment Unit and Paediatric ED.
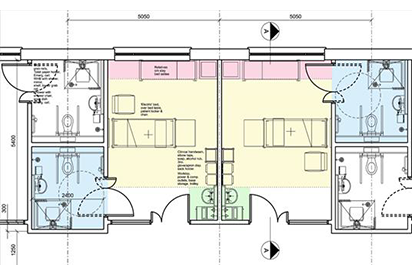
The Paediatric Assessment Unit should be equipped to cater for all ages from new-born to adolescent. Figure 4.1 identifies a bay configuration from Basildon University Hospital.
Appropriate provision for adolescents will be important in the Paediatric area; e.g. a separate adolescents’ waiting area, and privacy for adolescents with mental health issues as well as for children with behavioural difficulties.
Note that children are always accompanied by a carer and rarely attend singly, with extended family groups not uncommon.
4.2.1.7 Urgent Care Centre
An Urgent Care Centre (UCC) will treat Minor illnesses and injuries. This will include all patients who are able to self-present at hospital with injuries such as minor breaks, sprains and wounds. Triage / Initial Assessment will identify whether the presented condition is Major / Emergency, with the patient being redirected to an alternative pathway as appropriate.
4.2.1.8 Digital Delivery
The administration of medicines by nursing colleagues is best done digitally in Treatment Cubicles. The use of Information Technology (IT) facilities should not require colleagues to turn their backs on patients.
4.2.2 Key Themes of ED
The following are some of the key themes identified during clinical workflow engagement around the ED:
- Clear and accessible entrances are required, readily visible from vehicular and pedestrian approach routes with prominent and legible signage to indicate the intended use of each;
- Access routes for patients arriving by ambulance must be fully covered from vehicle to entry into the building;
- The Main Reception point should be readily visible and clearly identifiable from each entrance point;
- An initial ‘front of house’ assessment facility is required to enable all patients entering the ED to be streamed;
- Waiting spaces for patients and their families / carers should be attractively designed with access to natural light and views of soft landscaping and with a range of chair types, sizes and heights to suit varying needs;
- Good observation of all areas is essential to ensure the safety and wellbeing of all patients, their families / carers, and colleagues;
- Clear and intuitive wayfinding is required for patients and their families / carers with clear views of main access / egress points and routes supported by prominent and legible signage (including relevant graphics and symbols to aid those who have visual impairment, difficulty reading text or for whom English is not their first language);
- The boundaries between ED sub-departments should be capable of “flexing” to allow for fluctuations in patient numbers;
- Whilst Paediatric and Adult ED Waiting and Treatment areas must be segregated, ready access between the two areas will be required for colleagues;
- Any associated Assessment and Urgent Care facilities should be located immediately adjacent to the ED to enable patients to be moved quickly and efficiently into the appropriate care pathway;
- Dedicated Imaging facilities should be located immediately adjacent to Assessment and Treatment areas to enable intuitive patient and carer access without colleague assistance;
- Chair-centric and couch-centric Treatment cubicles must be capable of flexibility in use. The inclusion of fully glazed, easily operated sliding cubicle doors incorporating interstitial blinds to provide visual and acoustic privacy (essential for patients and their families / carers to have confidential and potentially distressing conversations with colleagues) is preferred;
- “Point of Care” testing facilities are required within the ED to provide a rapid diagnosis service;
- If designated as a receiving centre for major trauma and chemical incidents (as CRH already is), a permanent Decontamination Unit (rather than a tent type facility) comprising an Isolation Room with Gowning Lobby is required to deal with contaminated or infected patients without the need to temporarily close down other parts of the associated ED;
- A number of rooms with good observation and compliant with Royal College of Psychiatry recommendations will be required for patients with mental health issues. To ensure the availability of appropriate accommodation at all times, the possibility of making all cubicles suitable for mental health use through the introduction of manual pull-down shutters to conceal equipment (Nottingham University Hospital model) should be considered. All cubicles should be designed to be “ligature-light”;
- Good access is required to Operating Theatres and Critical Care to enable the rapid transfer of patients. Consideration should be given to the provision of dedicated lifts if these facilities are on a different floor to the ED;
- EDs and Pharmacies should be in close proximity;
- Sensitively designed accommodation is required for bereaved relatives in discrete but accessible locations, each such suite comprising a shared Waiting area with beverage preparation facilities and two separate private rooms offering high levels of visual and acoustic privacy;
- A Paediatric ED will be required to accommodate children of a wide age range from birth up to 18 years old and as such will require careful consideration of the varying environments, room layouts and equipment required to deliver emergency services in an age-appropriate, supportive and effective setting;
- Attractive working environments that support wellbeing are essential for colleagues who will be working under busy and often stressful conditions. As a result, access to natural light and ventilation, and external views are important together with adequate environmental control. Facilities must be provided for colleagues’ “downtime” in close proximity to but separate from clinical areas together with spaces for colleagues who may require emotional support in a confidential environment as a result of traumatic experiences;
- There are significant storage requirements associated with an ED and appropriately sized, equipped and located Stores are therefore required to ensure the efficient delivery of clinical services.


4.3 Surgery and Theatres
4.3.1 Operational Functionality of Surgery and Theatres
The Trust recognises that the opportunities to expand the established Operating Departments in their current locations will be highly constrained and, as a result, the current functions of the existing accommodation will remain unaltered. In line with the Trust’s Transformation Programme the nature of the surgical procedures to be undertaken at each site will change; a high proportion of elective services, that are currently delivered at CRH will be transferred to HRI with Trauma Surgery, Urology, Acute Emergency work and some plastic surgery transferring to CRH. In addition, complex planned surgery requiring Critical Care or Inpatient surgical beds, or involving higher risk patients with co-morbidities, will continue to be undertaken at CRH.
As a result, innovative and complementary alternatives should be explored; for example, supplementing the Emergency Theatre in the Maternity Department at CRH with an additional Theatre would provide the capability for both Departments to flex when in response to demand.
There are established operational benefits to providing a connection between the Operating Department and the Emergency Department. Consideration should be given to how such a link can be created, especially where the Departments are not co-located or physically adjacent to one another.
The existing Operating Department includes a variety of ‘soft’ spaces that are used for support accommodation, administration and outpatient facilities and there is recognition that augmenting / remodelling such spaces could lead to a more efficient use of these specialist areas. Returning the spaces to their originally planned use may help to accommodate the increased throughput and higher acuity of patients.
In line with the Trust’s vision to provide an exceptional working environment for colleagues that promotes wellbeing, opportunities to expand and improve existing changing and rest facilities should be exploited.
The planning of new Theatres should consider the benefits, in terms of flexibility in use, through the provision of laminar flow ventilation and radiological protection as well future developments in surgical procedures. In addition, whilst the Trust does not currently perform robotic procedures future designs should not preclude their introduction in the future.
4.3.2 Key Themes of Surgery and Theatres
- Operating Departments are required to enable the delivery of high-quality surgical procedures in a precisely controlled, functional and efficient clinical environment. However, the design should ensure that the internal environment supports wellbeing through the use of colour, finishes and detailing that provides an attractive, calming and non-institutional environment;
- Access to natural light is required in the Operating Department accommodation and this is of particular importance in the Operating Theatre and rest facilities for colleagues;
- Access to the Common Room spaces should be available in compliance with the BMA ‘Fatigue and Facilities Charter’ and these should be located on each floor so that they are accessible to all colleagues;
- Storage should be located logically, and close to the point of use thereby minimising travel distances for colleagues and ensuring that essential equipment and supplies are easily accessible when required; and
- 24-hour access to a flexible multi-purpose training and work space within, or close to, the Operating Department would be very beneficial for colleagues.

Source: Broadgreen Hospital, Liverpool.
4.4 Inpatient Wards
4.4.1 Operational Functionality of Inpatient Wards
Inpatient Wards should be sized to accommodate bed numbers that can be operated and staffed efficiently. In order to optimise flexibility, the design of Inpatient Wards should be based on a common ‘template’, that is readily capable of adaptation to suit the specific patient numbers and activity space requirements of different specialties.
The disposition of Wards and their individual layouts should enable the boundaries between them to ‘flex’ such that bed numbers can be correspondingly adjusted in response to changing operational requirements. For example, this will form a key part of the development of the layout for the floorplates of the expansion at CRH, together with the size and format of the bed spaces that make up the individual Wards.
The design of Wards should facilitate the separation and zoning of patients into clinical groups in response to seasonal variations in activity, case mix, and practice and to deal with infectious conditions.
Wards should be designed to function as discrete units and not as thoroughfares or as access routes to other wards or departments, unless dictated by specific clinical requirements.
An initial Ward size of between 24 and 28 beds is viewed as providing the optimum capacity, although this should be assessed on a case by case basis, reflecting the clinical speciality, as part of the design process of future projects.
The balance between single bedrooms and multi-bed bays is an important aspect of the design of the Ward accommodation and requires a wide range of factors to be considered. Notwithstanding the NHSI requirements for a minimum of 50% single bed accommodation patient privacy and dignity, observation by clinical and nursing colleagues, patient peer support, family space, infection control, access to sanitary facilities, and impact of noise on patient recovery should all be considered in conjunction with the general layout of the Ward.
The Trust has successfully adopted a decentralised model of nursing in some wards at HRI. The model utilises ‘touchdown’ bases for groups of patients numbering between 6 and 8 and is supported by localised storage of clinical supplies. The ongoing vision is that this will continue, forming the nursing model for new wards at CRH and will be supported by monitoring technology.
Wards should incorporate adequate space for clinical and therapeutic activities, and should promote social interaction between patients, families / carers, visitors and colleagues, whilst also providing spaces for reflection and ‘time-out’. A range of support accommodation may include, but not be limited to, Treatment Rooms, Family Rooms, Interview / Quiet Rooms, Ward Reception, Visitor Waiting, Patient Dayrooms, Administration, Clean & Dirty Utilities and Storage Rooms. The aspiration is that the layout of all Wards will become familiar to colleagues, which will facilitate flexible use by different clinical specialties when necessary.
Accommodation such as Relatives Overnight Stay, Discharge Lounge, the Junior Doctors' Room and multi-discipline Common Rooms will achieve greatest occupancy when the facilities are shared across a number of adjacent Wards.
4.4.2 Key Themes of Inpatient Wards
- The design of single bed rooms and multi-bed bays should be influenced by biophilic principles being comfortable, attractive, light, airy, offering appropriate patient privacy (visual and audible) and dignity, with external views from beds, preferably of distant vistas, soft landscaping or landscaped courtyards;
- All rooms should be adequately sized and optimally laid out to accommodate clinical activity, therapy and associated equipment and mobility aids without the need to reposition furniture. Layouts should discourage bed-bound inactivity. Enhanced patient bedside clothing storage would encourage patient mobility;
- Single bed rooms designated for bariatric patients, should have integrated hoists, and adequate space for associated equipment and manoeuvrability;
- All bed spaces should be designed to accommodate advances in digital technology;
- Adequate access to daylight is necessary to help patients maintain circadian rhythms and a sense of time;
- Individual bedside patient control of blinds should be provided to give patients a degree of control over their immediate environment;
- Individual bedside patient control of artificial lighting should be provided. A variety of lighting options will suit various clinical and patient activities, as well as provide opportunities for minimising energy consumption;
- Opportunities should be considered for patients to display pictures and other personal possessions, whilst complying with infection control requirements;
- A response should be provided to the increasingly important role played by relatives / carers in patient care. Incorporating overnight stay facilities in designated single bed rooms and offering relatives / carers opportunities for respite from the patient bedside whilst encouraging them to remain. In addition, overnight stay suites are required for relatives / carers; this would be on a shared basis between Wards;
- Patient safety and reassurance should be provided through optimum line of sight to / from nursing colleagues;
- Accommodation within each ward should be provided and ring-fenced to allow colleagues to communicate privately with families / carers;
- Adequately sized and appropriately located ward storage is required to eliminate storage of equipment in corridors and prevent storage elsewhere, e.g. dirty sluice;
- Adequate office accommodation for Junior Doctors should be provided on each ward;
- Access to a multi-discipline Common Room should be available for colleagues at each ward floor level, in compliance with the BMA ‘Fatigue and Facilities Charter’;
- An area forming a small visitor reception should be provided in each ward, co-located or integrated with a Ward Clerk’s base. This would also incorporate a small waiting area; and
- Wherever possible, internal corridors should terminate at external glazing to help colleagues in particular to maintain a sense of time and external contact.


4.5 Imaging and Diagnostics
4.5.1 Operational Functionality of Imaging and Diagnostics
Imaging facilities provide an essential element in the clinical pathways of many patients and should be easily accessible to both inpatients and outpatients. In addition, a significant number of patients attending EDs require rapid access to imaging in order to assess potentially life-critical conditions,therefore close adjacency between EDs and Imaging facilities are essential. As a result of these potentially conflicting requirements dedicated Emergency Imaging Satellite Units are often provided either within or adjacent to EDs to avoid emergency use of diagnostic facilities within the main Imaging Department, which can disrupt planned use by inpatients and outpatients.
Some additional facilities are planned to meet increasing demand from the current cohort of patients at CRH prior to the reconfiguration and extension works, while further expansion of the Imaging Department will be required to meet the needs of the additional inpatients who will be located on the site following completion of the reconfiguration of CRH and HRI.
4.5.2 Key Themes of Imaging and Diagnostics
- CRH Specific - Recent and proposed expansion of Imaging facilities within the footprint of the existing department has resulted in the loss of accommodation for use by colleagues that should be replaced at a size appropriate to the new enlarged facilities. The required accommodation includes Changing and Rest facilities for colleagues and flexible Multi-Disciplinary Team space;
- The imaging facilities associated with the CRH ED and the main Imaging Department should be closely related to enable colleagues to work flexibly to meet fluctuating demands and to respond to emergency incidents;
- Waiting areas should provide a range of comfortable seating and spaces for those in wheelchairs with natural lighting and views of soft landscaping where feasible. Discrete spaces should also be provided for patients in beds and on trolleys, close to the Imaging rooms but screened from public view to ensure privacy and dignity for patients who may be distressed or seriously ill. Facilities for relatives and carers to wait in close proximity to Imaging rooms should be provided.
- Waiting areas suitable for children awaiting imaging should be provided;
- Changing Rooms for patients who are required to change prior to imaging should be designed to ensure that patients do not have to wait in an open public waiting area with clothed members of public. Changing Rooms should be sized and equipped to suit a range of users including those with protected characteristics; and
- Accessible WCs should be provided in close proximity to Waiting areas.

Source: Medstar Georgetown University Hospital.
4.6 Education and Training
4.6.1 Operational Functionality of Education and Training
Education and Training are key components in the delivery of high-quality healthcare services and support both recruitment and retention of colleagues. Whilst some training is undertaken close to or even within the clinical departments, there is considerable value in providing a range of well-equipped and flexible spaces within an Education and Training Centre. This allows colleagues to take part in both formal and informal training away from the pressures of clinical services delivery.
Education and Training is undertaken in a number of ways including traditional classroom teaching, lectures & presentations, interactive workshops, one to one sessions and private study together with ‘hands on’ clinical simulation with extensive use of IT and audio-visual equipment.
Education and Training Centres should comprise a range of training rooms together with a raked lecture theatre, library and knowledge base, clinical skills lab, a flexible dining area, a reception area, an out of hours facility and ancillary accommodation in an area that has an external entrance together with an enclosed link to the main Hospital.
As part of the proposed reconfiguration of the CRH site, the existing education and training facility may need to be relocated in order to optimise the development site for the planned new build extension. The Trust is required to provide such facilities on site at all times therefore temporary decant to an appropriate space or to temporary accommodation is likely to be necessary; off-site provision is not considered to be tenable.
4.6.2 Key Themes of Education and Training
- There is an increasing demand for training of colleagues with an associated increasing reliance on technology. In addition, there is a requirement for improved access to small spaces within which small video conferences and private study can take place;
- Spaces are required to be flexible and easily reconfigurable to accommodate varying numbers of participants and a range of engagement formats;
- There is an increasing reliance upon technology for education and training requiring a significantly enhanced capability for connecting a range of communication and display equipment through both WIFI and hard-wired networks and full coverage of all areas by both systems is essential;
- Out of hours access is required for colleagues both from within the Hospital and externally with appropriate secure access control:
- Storage for a wide range of furniture, specialist clinical simulation equipment and presentation equipment is required to enable flexible use of the adaptable spaces;
- A Simulation Suite providing flexible clinical simulation areas with an adjacent Control Room is required. This will require a range of supporting accommodation including changing facilities, an office, storage for specialist equipment, a clinical skills laboratory and a debriefing room.
4.7 Facilities and Support Services
4.7.1 Operational Functionality of Facilities and Support Services
The delivery of Hard Facilities Management (FM) requires facilities from which these services will be delivered, preferably located within or adjacent to the Main Hospital. The accommodation will provide workshops, maintenance, medical engineering, stores and offices, and facilitate the management of cleaning and portering services.
It is essential to the Trust that any new development is wholly interfaced in order to be monitored from a single point within the hospital; i.e. BMS, Fire Alarm Panel, security, CCTV, etc
The Trust intends to develop their preferred strategy for the future delivery of Soft FM Services across the estate, which will include details of how the proposed expansion at CRH will be aligned with the arrangements already in place in the existing hospital.
Any expansion of CRH will likely place additional pressures on the existing Stores and Waste facilities. It is anticipated that the increase in deliveries and collections will be managed through increased frequency, rather than increased capacity. However, reconfiguration of the existing facilities may ultimately be necessary to provide additional essential accommodation and / or maximise efficiency. Future development will need to consider the connections between new and existing Soft FM flows whilst meeting the Trusts aspiration for appropriate separation between patients and visitors.
Separation of waste is currently managed at source, with waste streams being removed to the Waste Disposal Room in each clinical area. Waste Disposal Rooms will need to provide the capability for 5 cages/bins to allow waste segregation into laundry, domestic waste, clinical waste, recycling and other.
The CRH site is relatively constrained making it difficult for articulated vehicles to access the grounds. This is currently managed by large deliveries being made to HRI, which are subsequently transported by smaller vehicles (7.5T, Vans etc) and is not expected to change. This includes Linen, Pharmacy drugs, dressing and IVs. Provision for such logistics should be included within any future CRH design.
The Pneumatic Tube System currently installed at CRH is used by the Pathology and Pharmacy departments. The expansion of CRH will require the system to be expanded or supplemented to establish a similar capability in the new building.
It is anticipated that the existing catering facilities and restaurant at CRH provide sufficient capacity to accommodate the increase in patient, visitor and colleague numbers from the planned expansion of the CRH hospital. This should be validated at design stage.
4.7.2 Key Themes of Facilities and Support Services
- A wide range of Facilities Management and Support Services are provided by a number of organisations across the Trust’s two sites and it is an essential requirement that these services are coordinated and integrated to ensure that efficient and consistent standards are maintained during and after the proposed service reconfigurations; and
- The impact of these changes will vary considerably between the various services with some spare capacity in the existing CRH providing space for expanded services while other services including Hard FM requiring additional space to be created.
4.8 Digital Delivery
In 2012, the Trust developed a Digital clinical systems strategy that planned to fundamentally change the way services were delivered in the Calderdale and Huddersfield region. Continued investment in new infrastructure such as the cross-site wireless network, improved IT facilities and more resilient data storage has enabled CHFT to become one of the UK’s most digitally mature Trusts, measured against NHS England’s Clinical Digital Maturity Index (CDMI).
This was formalised in the Trust's five-year plan for digital health.
The accepted model for measuring progress towards achieving a full Electronic Patient Record (EPR) is the Electronic Medical Record Adoption Model (EMRAM). In August 2019, the Trust achieved Stage 5, placing it well above the UK and European average for a Trust of its size. The Trust plans to improve this position with an ambition to reach Stage 6 in 2020 and is determined that all local health partners become fully integrated, ensuring that the digital breadth and usability continue to expand beyond clinical services.
The Trust’s vision is for digital to become mainstream; empowering colleagues to become confident, effective and smarter-working users of multi-purpose and multi-disciplinary hand-held devices. It is also aligned with the NHS Long Term Plan, which is to improve out-of-hospital, person-centred primary and outpatient care. Digital will be the key enabler requiring a ‘cloud first’ strategy to be implemented as systems and estates are redesigned to include all processes used by the workforce. Office 365 will provide colleagues with the capability to work from anywhere and allow them to deliver exceptional clinical care.
Our future digital considerations will include:
- clinical solutions;
- workflow and patient pathways;
- local healthcare systems;
- broader Integrated Care System (ICS) solutions; and
- corporate services.
Whilst at the same time our reporting systems, Business intelligence and Data capture will advocate organisation wide coverage adopting a number of principles that will focus on “getting it right first time”. The Knowledge Portal will continue to drive the standard requirement of as much information as possible.
Fundamentally, technology should not hinder our colleagues in carrying out either their clinical or corporate roles, it should support.
As part of the West Yorkshire Association of Acute Trusts (WYAAT), Calderdale and Huddersfield NHS Foundation Trust is in the process of implementing the ‘Scan4Safety’ GSI Compliance Standard.
4.9 Clinical Adjacencies
As part of the development of this Design Brief, and through the colleague engagement, key clinical adjacencies associated with the Reconfigured CRH site were established and are referenced above.
These adjacencies prioritise critical connectivity within Trust accommodation and seek to provide design teams with primary information which should act as a briefing for development.
Key functional movement requirements include:
- Emergency Departments must have direct external ambulance entrances and an external access point for ambulant users;
- Emergency routes to and from Emergency Departments (ED) must be as direct as possible and cross flows with outpatients and visitors must be avoided;
- Direct internal access is required to permit the efficient movement of patients between Emergency Departments, Radiology, Operating Theatres and Critical Care Unit;
- FM entrances should be provided away from main public entrances with vehicular waiting areas and materials storage areas concealed from direct public view. Central FM services should be provided away from patient, colleagues and visitor areas. FM services within clinical departments should be zoned to minimise cross flows with patients and visitors;
- Access to Mortuaries for the transportation of deceased patients must be discrete and not pass through publicly accessible areas.
5 Design Brief – Functionality
New developments at CHFT are likely to operate more intensively than the Trust’s existing facilities and services will generally be provided over longer hours, including many which will be delivered on a 24 / 7 basis. Greater team working and integration of services will permit an expansion of short-stay and "one-stop" services.
In addition, there will be greater integration with community-based services. Although many existing planned out-patient services will continue to be provided within existing accommodation, the focus of the majority of the Trust’s new developments will be on emergency and unplanned care at CRH where the considered integration of all services associated with such care is of critical importance. Future redevelopment of HRI will include the improvement and adaptation of existing buildings as well as a new build Emergency Department.
5.1 Healing Environment
New developments should engender wellbeing, raise the spirits of patients and their families / carers, and enhance the morale, productivity and retention of colleagues through the adoption of measures aimed at enhancing their "quality of life". Designs should aid therapeutic objectives through the avoidance of excessively clinical or institutional settings and instead, focus on the creation of healing environments.
The following key factors, which can offer significant benefits, should be considered;
- Access to views, particularly on to areas of high-quality soft landscaping;
- Access to natural light;
- Access to natural and controllable ventilation to minimise the environmental impact of air conditioning;
- Patient control over aspects of their environment such as privacy, thermal comfort, light and noise;
- Clear and intuitive wayfinding;
- Reduced levels of ambient noise, particularly at night; and
- Access to social and family support.
- In order to create optimal patient healing environments, designs should also embrace key design tools and approaches such as:
- Biophilic Design: the harnessing of an innovative and rapidly developing method of designing therapeutic spaces to address alternative patient groups and settings. Key elements include the manipulation of light, spatial permeability, air quality, sensory engagement, liminal spaces, organic shapes and forms, natural processes and patterns;
- The application of evidence-based research to the design of diagnostic, treatment and recovery environments; and
- "Do no harm" (Florence Nightingale): the clinical environments created must not be toxic to the health of patients and indeed, should actively support health recovery and wellbeing. Issues of mismedication, Hospital Acquired Infection (HAI) and medical errors should also be addressed through the adoption of specific design solutions including the selection of materials and components in conjunction with careful detailing.
5.2 Natural light and ventilation
5.2.1 Natural light
Whilst natural and artificial lighting should be appropriately balanced to achieve a high standard of environmental quality, designs should maximise daylight utilisation. To facilitate this, deep plan spaces should be avoided but where unavoidable, they should be animated by the penetration of daylight and sunlight into courtyards, or via rooflights / light tubes.
In principle, any room that will be occupied by a patient or colleague for longer than an hour at a time should have a window, albeit it is recognised that in some circumstances, this will not be desirable for clinical reasons.
The following issues should be considered:
- Natural and artificial light sources should be designed to avoid / minimise glare;
- Glare and solar gain should be controlled by the appropriate use of brise-soleil, louvres and blinds. Where blinds are used, consideration should be given to use of interstitial types;
- Changes in level should be well lit and abrupt changes in illumination should be avoided, unless necessary as a clinical requirement;
- Glare on internal surfaces (e.g. reception desks, signs and notice boards) should be avoided; and
- The extent of glazed areas, windowsill heights, privacy and security requirements will require special attention to Ground Floor areas in order to ensure the adequacy of daylighting and views out whilst maintaining privacy and security.
5.2.2 Air Quality
Building layouts / forms shall be conducive to natural ventilation solutions, thereby limiting, as far as possible, requirements for mechanical ventilation and air conditioning to spaces where such arrangements are required for clinical reasons or to address issues of poor air quality.
Natural ventilation should be provided except where:
- Levels of external noise are unacceptable;
- Safety or security would be compromised;
- Wind and rain exposure would preclude achievement of appropriate ventilation rates;
- Unpleasant smells are generated either inside or outside facilities;
- Where flows of unfiltered / unconditioned air are clinically undesirable / unacceptable;
- Areas are air-conditioned; and
- Natural ventilation is not functionally possible or desirable for other reasons.
- Air quality in all areas shall take account of occupancy levels, internal pollutants, heat gains, external pollutants and atmospheric conditions and shall be controlled to provide adequate comfort and fresh air levels appropriate to the functions of each departmental area.
- The design of ventilation systems should be such as to minimise the risk of cross-infection and minimise energy consumption.
5.3 Adaptability
In order to ensure that future change can be accommodated, the design should make allowance for design resilience in the following ways:
5.3.1 Change
An adaptability strategy that addresses how clinical and technological change will be accommodated should be considered as part of the development of any design. This should address how future phases of development can be accommodated as well as how parts of the facility could be repurposed or even decommissioned as required.
Departments that are particularly subject to change (in either design or size) in the medium to long term, as a result of changes in technology, systems of care, volume of work and efficiency include:
- Emergency Department;
- Operating Theatres and Interventional Radiology;
- Imaging; and
- In-patient Wards.
5.3.2 Expansion
Clear strategies for physical expansion (horizontally, as well as vertically) in both the short and long term must be considered. Such expansion opportunities should be incorporated as a logical extension of the overall organisation of the hospital and must be fully integrated with any site master planning strategy.
The proposed design of new facilities and their immediate site surroundings should avoid compromising opportunities for future development of the remaining site.
Any proposed access and site circulation strategy should be robust enough to allow for future expansion.
5.3.3 Floor Plates
Departmental layouts and circulation arrangements should be designed to allow everyday changes of use, activity and space.
5.3.4 “Soft” Departments and Space
The inclusion of “soft” departments and space (e.g. back-of-house administrative accommodation) adjacent to clinical departments that are likely to expand in the future should be considered in order to facilitate clinical expansion with minimum disruption and at limited expense.
5.3.5 Flexible Departmental Boundaries
Designs should enable the boundaries between departments to “flex” whilst still maintaining full accessibility. In particular, the design of wards, and their disposition on each floor plate should be such that bed numbers can be correspondingly adjusted in response to changing operational requirements.
5.3.6 Standardised rooms
Consideration should be given to the adoption of standardised room sizes and dimensions for appropriate room types in order to facilitate interoperability and future change by means of minimal alterations and at limited cost.
5.3.7 Co-ordinated Construction Methodology
A co-ordinated approach to design and construction including structure and envelope, Mechanical and Electrical (M&E) services, partitioning, ceilings etc should be adopted in order to optimise flexibility in future re-planning / change affecting Departmental and room layouts including the provision and positioning of services terminals and equipment.
5.3.8 Structural Strategy
The adopted structural solution should facilitate adaptation and expansion with limited disruption.
5.3.9 Engineering Services Strategy
The adopted strategy should ensure that the M&E services systems are laid out, sized and zoned to readily accommodate future change and expansion and in addition, designed to enable routine maintenance or alterations to be carried out with minimal disruption and, wherever practical, without the need to access clinical accommodation.
5.3.10 Climate Change
As referenced in 3.4 and 3.5 above, the Trust is focussed on creating facilities that support our future environment, both from an energy efficiency and sustainability perspective.
Future development should take account of the Trust’s climate change adaptation and mitigation plans, being resilient to more frequent and increased severity of extreme weather events, including overheating. Flood prevention and the potential need for sustainable urban drainage solutions should be considered.
5.3.11 Technology
The design should take account of potential future changes in medical and surgical techniques.
5.3.12 Information Technology
The design should consider the impact of the Trust’s ongoing move from paper-based systems to electronic storage systems and the increasing use of IT based medical equipment.
5.4 Security
Security should be an inherent and discrete part of any design but a holistic approach to security should be adopted in order to limit the need for more visible barriers. The Trust’s strategy is to keep those intent on committing a crime from being given the opportunity to do so.
In developing the design, reference should be made, but not limited to the Trust’s Security Strategy.
Design considerations should focus on:
5.4.1 Layout
Hospital facilities and their surrounding site(s) should include appropriate internal and external supervision and control points. Internal layouts should maximise passive supervision where the monitoring of patients and visitors is required for either health & safety and / or security reasons.
5.4.2 Access, Routes and Car Parks
The design of roads, footpaths and parking areas should consider the safety of patients, visitors and colleagues. Car parks and their routes to and from the hospital should be overlooked from buildings, be attractive and well lit, secure and be monitored by a high level of security, such as CCTV.
5.4.3 Landscaping
Landscaping design should be an integral part of the security strategy and the safety of all using the hospital site(s), whilst still providing an attractive environment. All external landscaped areas and accessible courtyards should be well lit and safe without compromising their design.
5.4.4 Minimising Entry Points
Entry and reception points should be minimised and should allow for natural supervision and / or monitoring of movement and entry / egress.
There should be a clear delineation between public and private areas both internally and externally. The number of 24-hour access points should be limited.
5.4.5 Minimising Potential Crime Areas
Designs should avoid recessed entrances and dead-end spaces and minimise isolated areas to reduce the risk of potential crime. Designs should also discourage the misuse of hospital sites for anti-social activities.
5.4.6 Lighting
External areas that will be used during the hours of darkness, such as ingress and egress points, drop-off areas, roads, pavements and car parks, should be appropriately lit to provide a secure, protective and attractive environment.
Good natural and artificial lighting should be provided to all internal areas.
5.4.7 Natural Barriers
Designs should consider the use of natural barriers, such as the depth of reception desks, to avoid the need for more overt security controls.
Designs will be required to incorporate equipment including CCTV cameras, access control equipment and alarm systems but should maximise opportunities for clear observation of entrances and eliminate concealed spaces.
5.5 Control of Infection
The Trust’s Infection Control team should be consulted and involved from the outset of any design, and its policies and HBN 00-09 “Infection control in the built environment” observed, so that all recommendations are designed into projects from first principles.
5.6 Fire
The fire strategy for every development should follow the requirements contained in Health Technical Memorandum (HTM) 05-02: "Firecode - Guidance in support of functional provisions (Fire safety in the design of healthcare premises) published by the Department of Health".
It is recognised however, that it is not possible for all eventualities to be captured within a single generic document. In arriving at design solutions, any proposed deviation from the requirements laid down in HTM 05-02 must therefore be discussed and agreed with the Trust’s Fire Safety Advisor, Building Control and the Fire Authority.
5.7 Privacy & Dignity
Designs should accommodate the requirements for privacy and dignity of all who will use the facility. Reference should be made, but not limited, to "The NHS Constitution".
Design Measures should include:
- Provision of in-patient accommodation in minimum 50% single bed rooms with en-suite facilities;
- Good visibility of patients by colleagues and of colleagues by patients;
- Privacy control to doorset vision panels and glazed screens to all clinical and patient rooms and to other areas as appropriate;
- Provision of appropriate sub-waiting areas including, as required, separation of male / female and dressed / gowned patients;
- Adequate provision of changing, washing and WC facilities for all colleagues;
- Appropriate facilities for visitors including access to services to provide the optimal patient and public experience; and
- Specific provision for the discrete transportation of bodies to Mortuaries.
5.7.1 Acoustic Privacy
In order to ensure comfort and appropriate levels of privacy for patients and colleagues, acoustic performance should meet the requirements defined in HTM 08-01 “Acoustics”.
Particular attention should be paid to areas such as:
- Clinical examination and consultation rooms;
- Confidential areas such as reception desks etc. where patient and other confidential information is discussed;
- Patient bedrooms and en-suite sanitary accommodation;
- Teaching / seminar areas; and
- Interview Rooms.
A programme of funded research and improvement work at Calderdale and Huddersfield NHS Foundation Trust, led by Professor Felicity Astin and team, has informed a series of recommendations presented in a report entitled “Promoting Sleep and Rest for Patients in Ward Settings: A Quality Improvement Initiative at Calderdale and Huddersfield NHS Foundation Trust”. The study recommendations will be considered in the development of new or refurbished accommodation within the Trust.
Attention should also be given to the design of engineering systems to minimise the generation of excessive noise. Provision should be made to minimise the transmission of plant noise and vibration, and distribution systems should be configured to minimise the creation of regenerated noise within occupied areas. The installation of services through the building fabric must not compromise the acoustic performance of such elements in any way. Where necessary, additional attenuation or acoustic isolation provision should be included.
5.7.2 Visual Privacy
Consideration should be given to:
- The provision of discrete waiting areas that are not part of a larger circulation space. Colleagues should be able to observe patients without them feeling overlooked;
- Visual screening to inpatient and treatment areas where patients are in distress or partial undress;
- Windowsill levels enabling outward visibility for patients in wheelchairs or beds without compromising patient privacy;
- The provision of interstitial blinds to door vision panels and glazed screens to bedrooms and clinical areas.
5.8 Supportive Environments
For those living with challenging behaviours including learning difficulties, dementia and autism, understanding their surroundings is fundamental. Designs should therefore respond to three
categories of impairment, sensory, cognitive and physical, creating environments which appropriately balance the need for constructive sensory stimulation with that for calm reassurance. A supportive and therapeutic design strategy should therefore be developed, aimed at:
- Providing a safe environment;
- Providing optimum levels of stimulation;
- Providing optimum lighting and contrast;
- Creating a non-institutional scale and environment;
- Supporting orientation;
- Supporting wayfinding and navigation;
- Providing access to nature and the outdoors;
- Promoting engagement with relatives, friends and colleagues;
- Providing good visibility and visual access;
- Promoting privacy, dignity and independence;
- Providing good wheelchair access;
- Providing gender neutral toilets;
- Promoting noise reduction and attenuation;
- Promoting physical and meaningful activities; and
- Supporting diet, nutrition and hydration.
5.9 Access
Designs should adopt an integrated approach to access such that clear and intuitive routes for patients and their families / carers are available and colleagues are readily able to access their places of work. Journeys onto hospital sites, from pedestrian / vehicular routes, through main receptions, into the hospital and to the desired end locations should follow a safe, logical, clear and intuitive system.
5.9.1 Access for All
Designs should accommodate the needs of people with disabilities including, but not limited to wheelchair users, frail people, those with poor mobility, those who are hard of hearing or sight impaired and those with mental illness. Reference should be made, but not limited, to:
- • Building Regulations Part M;
- • Health Building Note 00-04 “Circulation & communication spaces”;
- • BS 8300-1: 2018 and BS 8300-2:2018; and
- • Disability Discrimination Act (DDA) or Equality Act 2010.
Consideration should be given to the use of automatic doors to improve access into and about facilities for those who are wheelchair bound, have reduced mobility or are visually impaired.
Designs should provide secure wheelchair parking and power / battery recharging for disability vehicles.
Appropriate technologies for people with disabilities, such as induction loops to entrance and reception areas and emergency call systems in areas such as toilets and bathrooms, should be incorporated.
The Wayfinding strategy should be accessible to people with disabilities.
5.9.2 Vehicular access
Vehicular segregation including separate emergency ("blue light"), goods / services vehicles, patient / visitor / colleague and public transport routes should be considered as part of site-wide access strategies.
5.10 Space
The functional content and spatial requirements for each new development will need to be developed in collaboration with the Trust.
Rooms should be of appropriate proportions and should not incorporate acute angles, curves, columns or the like where these would preclude effective use of the space.
5.10.1 Circulation, Lifts & Stairs
Appropriate provision, including waiting / sub-waiting areas, should be made for the movement of patients, pedestrians and the transportation of goods, food and waste. Account needs to be taken of varied means of patient transportation; i.e. on foot or by wheelchair, trolley or bed (with surgical attachments).
Doors and lifts are required to be of a width and length to allow wheelchair access and the transportation of mobile medical equipment; e.g. x-ray machine, supplies, linen trolleys, patient trolleys and beds with surgical attachments.
Lifts should be able to accommodate large numbers of patients together with those escorting them, e.g. relatives and / or clinical / support / portering colleagues, potentially with multiple pieces of mobile and fixed equipment. Dedicated bed and FM lifts should be provided, to separate services from passenger transport.
As a minimum, the dimensions and planning of circulation routes should satisfy the recommendations defined in HBN 00-04 "Circulation and communication spaces".
5.10.2 Storage
Adequate facilities for clinical storage and supplies should be readily accessible and secure. Early consideration should be given to the use of different storage systems, such as HTM 71 type modular storage and intelligent storage, as a means of enhancing storage efficiency.
5.10.3 Public Spaces & Entrance Areas
Adequate space should be allowed around reception desks and waiting areas to accommodate users without obstructing circulation flow.
Consideration should also be given to the inclusion of space to allow for informal discussion and interaction within public areas and to making use of open areas within clinical areas as "break out" space.
5.10.4 Wards
Ward layouts should:
- Meet or exceed the standards of space and environmental quality contained in NHS Estates guidance. Adequate space should be incorporated for clinical and therapeutic activities, teaching, medical equipment and visitors within patient bed areas;
- Ensure appropriate patient privacy and dignity; and
- Facilitate the separation and zoning of patients into clinical groups in response to seasonal variations in activity, case mix, and practice and to deal with infectious conditions.
5.10.5 Courtyards
Courtyards should be well designed to provide visual amenity and provide a link between external and internal spaces, assist in wayfinding and serve as a source of natural light and ventilation. As such, they will potentially be an important element of any design. Access to courtyards for maintenance purposes, including window cleaning, should be from public circulation areas.
5.11 Wayfinding
The Trust’s existing estates are large, extensive and can be confusing. With further developments, enabling patients and visitors to reach their destination from when they first arrive, at a time when they may already be stressed, may potentially be problematic and even distressing for people. An effective Wayfinding strategy will therefore be essential.
Such a strategy should be integrated with Interior Design and Arts strategies, enabling patients, visitors and colleagues to orientate themselves with ease around and within the hospital and its immediate site utilising a comprehensive directional system comprising landmarks, artworks and clear signage, both externally and internally. The Wayfinding system should also create reference points for colleagues to direct patient flows with clarity and simplicity.
Patterns of site movement from all points of arrival must be logical, clear, intuitive and unambiguous for patients, visitors and colleagues, minimising travel times and distances. Specific consideration should be given to first impressions created at the entrances to the site and approaches to buildings.
The disposition of internal spaces must be clear and coherent with appropriate space provision allocated for circulation and waiting / sub-waiting spaces, all with the objective of facilitating the safe and effective movement of patients, visitors and colleagues, and the efficient transportation of goods and waste materials.
Signage should support, but not be the prime method of indicating movement patterns. The wayfinding strategy should create focal points throughout the site, recognising patients’ varying needs at points in their journeys.
6 Design Brief – Character and Innovation
6.1 Overarching Design Ethos
New developments should in themselves serve as demonstrations of the value of good design, and how it can improve the lives of patients and colleagues and deliver added value for the Trust.
Designs should address the following issues and opportunities:
- The therapeutic impact on patients of good design;
- The influence of good design in the creation of positive, high quality working environments for colleagues;
- The reassuring impact of good design on patients and their families / carers;
- The impact of good design on overall colleague satisfaction and recruitment / retention;
- The role of design in maximising flexibility;
- The potential for improvements in clinical efficiency and effectiveness;
- Opportunities to reduce energy consumption and carbon emissions, and to improve sustainability;
- Opportunities to increase the efficiency of non-clinical services; and
- Opportunities to enhance patient safety including maximising the effectiveness of infection control measures.
6.2 Citizen Satisfaction
6.2.1 Orientation
In ensuring that developments respond appropriately and effectively to their specific orientation on site, the following should be considered;
- Solar heat gain, solar radiation and glare on the design of the external envelope;
- Views of the development from surrounding areas;
- Views out from the development, including the implications of overlooking of adjacent properties;
- Views out from the development into courtyards, including their design, dimensions and proportions;
- Prevailing winds and their effect, in conjunction with the development, on surrounding areas;
- The impact of traffic noise on the design of the development’s external envelope;
- Landscape design, including plant selection, relative to the orientation of landscaped areas around the development and within any internal courtyards; and
- The impact of varying site levels across the site and their potential use to zone the building and achieve an appropriate separation of patient, visitor and FM flows.
6.2.2 Scale and Proportion
The scale and proportion of developments should relate both to their immediate site context and wider urban / suburban location. Proportions and scale should reflect those of retained existing buildings as well as those of adjacent properties. Irrespective of the size of the development, scale should be considered from the point of view of patients, visitors and colleagues to ensure that developments appear welcoming and approachable.
6.2.3 Composition
The design of new developments and their immediate sites should present pleasing and well composed building forms that contribute to their environments. The overall composition of developments should enhance their sites and create a sense of place. In doing so, the following issues should be considered;
- The massing and height of the component parts of developments relative to the whole and to the topography of their sites;
- The profile and skyline of developments when viewed from a distance and on approach;
- The individual components of overall compositions;
- The interplay of light and shadow in adding definition to the built form;
- The balance between solid and glazed elements;
- Consistency, clarity and attention to detail; and
- The considered integration of services elements such as plantrooms, flues, cabinets, grilles and rainwater pipes.
6.2.4 External Materials
The selection of external materials and cladding should enhance developments as a whole, contributing to the achievement of appropriate design solutions in terms of quality, scale, colour and environmental requirements. Materials should be of high quality, durable, economical and easily maintained over their lifespan.
In selecting external materials, the following should be considered:
- Materials should be well detailed, appropriate to the relevant site and surrounding buildings and remain visually attractive throughout their life;
- Materials should be durable, weather well and be easy to clean, maintain, repair and replace as necessary;
- The selection of materials should take account of sustainability concerns; and
- External cladding materials must conform to all current and anticipated safety and statutory regulations.
6.2.5 Colours & Texture
Appropriate use of colour and texture should be made both externally and internally to articulate and enrich the form and appearance of developments.
Externally, the use and choice of colour and texture should be considered in relation to surrounding buildings, the overall form of any development and appropriateness to its location.
Care should be taken to ensure that developments, by virtue of the chosen colour(s) of materials, do not date. Rather, the selection and use of colour(s), whilst being contemporary and modern, should ensure that developments age gracefully and elegantly.
Consideration should be given to the use of colour to help create an immediate and distinct development "image" which is interesting and stimulating. Colour can also be used to identify entrances and routes, thereby enhancing wayfinding.
6.2.6 Views
Designs should provide pleasant views from patient, public and colleague only areas. These should ideally be out on to surrounding landscape / environment or into enclosed landscaped courtyards, reflecting evidence that patient wellbeing is enhanced, and recovery times reduced where such views are available. Views on to active areas will enable patients to be aware of people around them, distracting from their medical condition and reducing any sense of isolation within the hospital environment.
Provision of the following views should be considered;
- From all patient areas where possible, but especially from patient bedrooms. In this respect, accessibility of view should be considered in the detailing of the building, e.g. the level of window sills relative to a bed-bound patient;
- On to external areas or adjacent internal public areas from waiting areas to provide distraction and pass time in these areas;
- From internal public areas on to external areas reinforcing connectivity with the surrounding area and aiding wayfinding;
- On to elements or areas at ground level or elements at higher levels such as surrounding buildings, the tops of trees etc;
- Short, into enclosed courtyards, or longer, across adjacent rooftops;
- Carefully balanced with views into spaces from outside that might otherwise compromise patient privacy and dignity. In particular, the design of ground floor rooms should consider aspects of privacy and security;
- Into internal spaces, e.g. of the waiting area to clinical facilities from an external entrance, enhancing natural wayfinding; and
- From public circulation areas, such as a hospital street / main communication route and lift / stair cores either on to external areas of the hospital or into enclosed courtyards, reinforcing patient / visitor orientation.
6.3 Internal Environment
Designs should create high quality, ergonomically satisfactory internal environments which facilitate delivery of a high standard of professional care with ease and dignity, and provide reassuring and safe environments for patients, their families / carers, and colleagues. Interior environments should:
- Incorporate welcoming and pleasant main / departmental entrances and reception areas;
- Have a calming and non-intimidating appearance;
- Provide reassuring and comfortable patient areas;
- Incorporate stimulating and interesting public areas;
- Include attractive and efficient areas for colleagues including relaxing rest facilities;
- Maintain comfortable temperatures in all seasons and air quality that is fresh; and
- Provide acoustic performance that supports individual privacy and dignity.
A coherent interior design strategy, integrated with the overall vision for the respective hospital, should be adopted for each development. Issues requiring consideration include:
- Materials and finishes should complement departmental layouts in order to create varied environments that respond to the nature of the specific spaces and their functions, but within a coherent overall strategy;
- The form, scale, colours and overall appearance of furniture and fittings and colours of finishes should be well co-ordinated, timeless and designed with care to avoid any sense of clutter or disorganisation. Robustness, durability and ease of construction must not be achieved at the expense of scale, aesthetics and the creation of a humane environment;
- The selection of finishes must take account of infection control issues;
- The Interior Design strategy should be fully integrated with Wayfinding and Arts strategies;
- The focus of the interior design process should be on key design features that will have a significant impact on building users in order to ensure effective use of financial resources.
Extensive consultation with user representatives should be undertaken at appropriate points in the design process to ensure the design solution is responsive to their specific requirements, both operationally and aesthetically, as well as maintaining the corporate requirements of the Trust.
6.4 Patient Environment
Internal environments should be comfortable, relaxing and reassuring for patients. In addition, clinical areas must be of a technical standard appropriate to the services to be delivered.
Communal patient areas such as day rooms and interview rooms should be human in scale and ambience. Public areas such as waiting, and reception areas should be restful, open and non-threatening.
Patient bed areas should provide a non-institutional environment with unobtrusive and calming lighting and be designed to ensure patient privacy and dignity.
Designs should create welcoming, reassuring and open environments, but ensure privacy for patients and their visitors when required. The following features should be incorporated:
- Good visibility of patients by colleagues and of colleagues by patients;
- Privacy control to door vision panels and glazed screens to all clinical and patient rooms and to other areas as appropriate;
- Windows that maximise the provision of daylight without glare, with sill levels which enable outward visibility for patients in wheelchairs or beds without compromising patient privacy, and, where clinically appropriate, provide natural ventilation whilst maintaining a safe and secure environment and taking account of the tactile and thermal sensitivity of patients;
- Facilities should be designed to ensure compliance with the commitments laid down in “The NHS Constitution”;
- Where practical, non-clinical areas should be provided close to Departmental entrances to limit incursion into clinical areas;
- Reception points should be readily visible and accessible to patients and should facilitate dialogue with users at varying heights, e.g. at low level for children and wheelchair users, whilst maintaining colleague security and patient privacy during the transfer of information.
6.5 Public Environment
There should be a clear distinction between public and private spaces, and this must be integral to the Wayfinding strategy and signage solutions.
Public waiting and meeting spaces should appear light and spacious. They should be capable of use for a range of activities including health promotion events, fundraising, exhibitions and performances. In order to permit intuitive orientation, they should not be repetitive, and should provide a focal point for the provision of information.
Public spaces should be used to integrate the various parts of a hospital, and should avoid appearing as spaces joined by long, narrow corridors. Some spaces should be designed to encourage social interaction for patients, colleagues and public whilst others should provide an environment to support quiet and reflection for relatives of patients.
6.6 Working Environment
The provision of high-quality working and rest facilities for colleagues is a high priority for the Trust and in addition to the facilities already available, it is committed to the provision of ‘mess’, rest, study and changing facilities in compliance with the recommendations of the BMA "Fatigue and Facilities charter".
6.7 Urban and Social Integration
6.7.1 Sense of Place
In order to maximise their civic qualities, cognisance should be taken of the nature of each specific development site and the impact of new developments on their individual sites and wider contexts.
A “sense of place” should be created through the considered interaction of new developments, existing retained buildings and the spaces between buildings.
The arrangement of routes, both internal and external, pedestrian and vehicular, connecting developments to the rest of their sites and surrounding roads will be vital in achieving successful design solutions.
6.7.2 Good Neighbour
New developments should be designed to complement and enhance the quality of the locality in which they are located, i.e. be regarded as a "good neighbour". They should be welcoming, inclusive and vibrant. They should facilitate easy access by the communities and groups who will use them and should reflect the objectives of the Trust in the regeneration of its healthcare facilities.
In developing designs, the following issues should be considered;
- Developments should be sensitive to their relationships with their surroundings and overall visual impact, particularly if located in a Conservation Area, thereby enhancing their context;
- The height, massing and skyline of developments, particularly in relation to adjacent (especially residential) areas, should be given careful consideration;
- Public and private areas should be appropriately defined;
- Views of service areas and other more “industrial” parts of developments should be screened from public entrances, adjoining public spaces and surrounding external areas; and
- The selection of external materials should pay due regard to neighbouring developments.
6.7.3 Contribution to the Community
The Trust’s existing hospitals are significant elements of their local communities in terms of physical size, as providers of a wide range of acute healthcare services and as major employers.
Developments should therefore continue to encourage a sense of community within the hospitals themselves and within the communities they serve. Designs should also promote the integration of the hospitals with the wider communities of which they are part. Some of the patient communities served experience high levels of social deprivation and unemployment but are rich in cultural and ethnic diversity. Developments should celebrate these varied communities.
Developments should contribute to the community by:
- Reinforcing civic pride through the creation of landmark buildings;
- Enhancing their contexts;
- Taking account of the cultural diversity of the local population;
- Providing amenity spaces, within and around them, that can be used by the community; and
- Improving the quality of surrounding public spaces.
6.8 Innovation
Designs should reflect current and developing innovations in the delivery of healthcare services and design of healthcare facilities. Innovation in design can range from the micro to the macro, e.g. concepts of whole hospital planning, the distribution of functions and the detailed design of components, spaces and use of technology.
Designs should explore innovation in clinical practice / techniques and built form. Developments should reflect new models of healthcare provision and respond to advanced thinking about master planning, architecture and the built environment.
6.9 Art
The provision of artwork within healthcare environments is now recognised as a key component in the creation of a successfully designed interior. Art themes can complement the Interior Design Strategy by intrinsically linking buildings together through a common use of patient focused artworks. Art themes can also assist the Wayfinding Strategy. The introduction of natural light, the use of materials and texture and the application of colour are associated concepts that can enhance the arts strategy.
The inclusion of art within and around the CHFT hospital estate is a key opportunity to integrate with and involve the local community, from commissioning local artists to involving local school children and patient groups.
7 Design and Construction Standards
Design solutions should achieve excellence in all aspects, from master planning and external landscaping, to external and internal appearance. They should express clarity and coherence and, in combination with appropriate massing, scale, form, materials and colour, result in developments of enduring high quality which age well, retain an attractive appearance over their lifetime and convey a positive image of the Trust, reflecting the standards of excellence the NHS aspires to achieve.
7.1 Build Standard
7.1.1 Durability
- Facilities should be able to withstand wear and tear in use without unduly exhibiting obvious damage or requiring excessive maintenance or repair; and
- Finishes, components and assemblies should be easy to clean, maintain, repair and replace as necessary and should remain visually attractive throughout their life.
7.1.2 Robust Construction
- Materials finishes and forms of construction should be robust and durable. The selection and specification of materials and finishes should be appropriate to their location and function, and the detailing of junctions between materials and components well considered.
7.2 Repeatable Designs, Standardisation and Prefabrication
Appropriate consideration should be given to the use of ‘repeatable’ room types whilst constructional design should exploit the use of standardised and prefabricated elements where this can make construction faster, more efficient and / or more affordable and / or offer a higher quality or more sustainable solution.
7.2.1 ‘Repeatable’ room types
In order to reduce design time / costs and limit the required input from clinical and nursing colleagues, consideration should be given to the use of tried and tested ‘repeatable’ room types such as those developed through the "ProCure22" framework and to the development of further rooms specific to the Trust’s requirements.
7.2.2 Generic rooms
Consideration should be given to the use of "generic" / standard rooms, flexible multi-purpose room types equipped on a "loose fit" basis to deliver a wider range of clinical services, thereby achieving Capex and Opex savings through increases in occupancy and a consequent reduction in the overall number of rooms required.
7.2.3 Standardised Elements
Standardisation should be applied to repeat elements to benefit operational requirements and maintenance. However, such standardisation should not compromise operational performance in any way and each element should be entirely compatible with each specific application.
Consideration of standardisation should include, but is not limited to, the following:
- Structural elements;
- Plant;
- Equipment;
- Lighting fittings;
- Bed head units;
- Sanitary appliances and assemblies;
- Door sets;
- Floorcoverings;
- Suspended ceilings; and
- Wall protections systems.
7.2.4 Prefabricated Elements
In order to take advantage of the repetitive nature of construction, maximise productivity and efficiency and minimise construction periods and waste, consideration should be given to off-site prefabrication.
Prefabrication should specifically be applied to repetitive elements, e.g. structural elements, bathroom pods, sanitary assemblies or complex equipment such as M&E plant assemblies.
7.2.5 Maintenance
Ease of maintenance, both internally and externally, should be a priority such that the replacement of services, finishes components, elements, systems, furniture and equipment can be carried out safely and effectively within the requirements of clinical operations and functionality.
7.3 Engineering Requirements
A building and engineering management system should be provided within the proposed development to control, monitor and protect all engineering and building systems.
Consideration should be given to the integration of various building and engineering systems such as automatic controls, sprinkler systems, lighting controls, building management systems, access control systems etc., in order to achieve a comprehensive coordinated system.
The design should provide an overall controls strategy that can demonstrate its benefit in the operation of the buildings to the Trust. The integration of building and engineering systems should be based on proven technology and the design and supporting documentation should demonstrate that such proposals can be achieved.
The following issues should be considered:
- Engineering systems should be flexible, efficient and economical in use, and in use of resources;
- Systems should look to minimise their impact on the environment through a coordinated plan in order to achieve a carbon neutral status;
- Engineering systems should be designed, configured and controlled to reflect the operational, occupational and variable needs of each department;
- Engineering systems should operate quietly;
- Controls for all engineering systems should be simple and easy to understand and operate;
- Local controls should be provided for use by colleagues and patients;
- Engineering systems for departments that are not operational 24 hours per day should facilitate the shutdown / set-back of systems, including ventilation, heating and lighting, for the appropriate period;
- Controls to turn off / set-back engineering systems that are not in use should be provided for all departments;
- An appropriate level of security and resilience must be provided to life safety systems, e.g. fire alarms, medical gas alarms; and
- An appropriate level of resilience must be provided to proposed integrated systems.
7.3.1 Primary Energy Plant and Equipment
The Trust are looking for all of their buildings to evolve over the coming years such that the installed systems have a lower impact on the environment. The use of fossil fuel-based engineering technology is to be challenged.
Schemes will need to consider low carbon or carbon neutral primary energy sources, along with site generation through renewable technologies, in order to best mitigate the production of carbon through the development.
7.3.2 Internal Lighting
The provision of artificial lighting to all spaces within the hospital is required. A detailed analysis of the functions of each type of space will inform a detailed lighting design strategy. The lighting design strategy should consider the following:
7.3.2.1 Therapeutic Benefits
The lighting design strategy should recognise the therapeutic benefits of good lighting and appropriate lighting should be specified for all spaces with particular attention paid to patient and public spaces.
7.3.2.2 To Support Wayfinding
External lighting should be designed to illuminate the entrances to, and routes through the site and the main entrance to the hospital itself. The external lighting should enhance security and be integral with the security and access strategy.
Inside the building, lighting should be used to guide the patient or visitor in the direction of the waiting area, to the reception desk where they can receive assistance.
7.3.2.3 Energy Consumption
The lighting design strategy should utilise low energy lighting, reliability and low maintenance. Furthermore, in public areas such as the main entrance, public circulation, waiting areas, cafeterias, different types of lighting that enhance and complement the interior design of the space should be used.
7.3.2.4 Appropriateness and accessibility of control systems
The control system for the lighting should be simple and easy to use and the controls and switches must be readily accessible. The control system should give patients, within their bedrooms or wards, local control over their immediate environment to enhance their privacy and dignity, whilst still providing sufficient operational levels of lighting for reading and for clinical functions.
7.3.2.5 Relative levels of task and background lighting
Lighting levels should follow guidance given in the relevant CIBSE Lighting Design guides for the various working environments. Minimum levels are defined in HTMs, HBNs and should be identified in Room Data Sheets along with any requirements for specialist task lighting.
7.3.3 Fire Planning
The clear fire planning strategy should be incorporated into the design in accordance with the requirements of HTM 05-02.
HTM 05-02, and the series of which it is part, provides specific guidance on fire safety in the design of new healthcare premises and major new extensions to existing healthcare premises. While not intended to cover every possible scenario, the standards and principles it advocates recognise that fire safety in healthcare premises is dependent on the interaction between physical fire precautions, the dependency of the patient, the fire hazards and the availability of sufficient and appropriately trained personnel to safely evacuate patients in a fire emergency.
The following issues are required to be considered:
- Fire detection and alarm system;
- Sprinkler systems;
- Separation of Hazards;
- High life risks potentially compromised by high fire loads;
- Means of escape - access and egress routes;
- Compatible security and door access controls;
- Signage; and
- Emergency lighting.
7.3.4 Heating Ventilation and Air Conditioning (HVAC)
Heating, ventilation and air conditioning systems should be logically designed to operate efficiently and provide local control as appropriate.
The energy and power systems are to be appropriately designed to provide fully integrated designs in terms of the incorporation of engineering services into the building fabric and external spaces.
Acceptable comfort conditions in all areas should be provided but this is particularly important in clinical areas and the design should demonstrate strategies for achieving optimum comfort together with minimum energy consumption. Whether ventilation and temperature control is provided via natural infiltration and heat emitters or all air mechanical systems, provision should be included for solar control measures to reduce heat gains and hence improve thermal comfort thereby minimising energy consumption.
7.3.4.1 Heating
The design of the heating system should include:
- Recessed pipework with access provided for maintenance;
- Appropriate access should be provided to enable the reading of sub-meters
- Location of heat emitters should be fully co-ordinated with building fabric and space planning;
- Individual sub-compartments with their own zoning system should be provided to optimise energy efficiency; and
- Individual room temperature control should be provided to all occupants in all rooms.
7.3.4.2 Ventilation
Natural ventilation should be utilised where possible but where mechanical ventilation is deemed necessary systems should incorporate energy recovery, zone control and be dedicated to specific areas of the building.
Ventilation serving clinical zones within the hospital should be on essential supplies supported by back-up generators to ensure that power failures do not interrupt normal operation of the respective areas.
Consideration should be given to night set-back and reduced air flows whenever appropriate to minimise energy consumption.
Specific ventilation requirements for infection control should be set out in output specifications, including the following key requirements:
- Ventilation should dilute airborne contamination by removing contaminated air from the room or immediate patient vicinity and replacing it with clean air from the outside or from low risk areas within the health care building;
- Air intakes must be located away from other air exhausts;
- Ventilation grilles should be designed so that they can be easily accessed for cleaning and do not attract dust and dirt; and
- Ventilation systems provided throughout the development should comply with all relevant HBN and HTM standards with specific reference to HTM 03-01.
The following are examples of specific departmental requirements which should be strictly observed:
- Isolation rooms should be provided with ventilation systems in accordance with HBN 4: "Enhanced single rooms with en-suite facilities";
- Theatre ventilation must be sufficient for the purpose of the theatre;
- Ventilation in Radiology departments must take account of the increasing amount of invasive procedures performed;
- Theatre ventilation standards will also be required in certain other specific areas e.g. cardiac catheter labs; and
- There will be a requirement for air conditioning / temperature control to be provided in any intensive care facility and isolation facility.
Consideration should also be given to provision of cooling to areas of high internal heat gain such as Renal departments.
7.3.4.3 Air-conditioning
Air-conditioning and / or comfort cooling should be provided to spaces with the established requirements described in the project requirements document and / or Room Data Sheets.
7.3.5 Hot Water and Steam Generation
The design of the hot water and steam distribution systems should consider and include appropriate equipment and isolation facilities to allow ease of maintenance.
Systems should include suitable provision of duplicate plant and allow standby capacity in the event of failure. Domestic hot water systems should be designed to provide adequate flow to satisfy maximum demand whilst minimising stored hot water and energy consumption. The provision of some storage is desirable to reduce the impact of hot water generation on boiler power.
The control of legionella and other bacteria within the system is critical and guidance in this regard is considered mandatory. Hot and cold-water systems should be designed in accordance with HTM 04-01.
Steam systems should be provided as required for process use, sterilisation and humidification. If steam is proposed as the primary heating medium, dedicated steam generators will be required for sterilisation unless the sterile services department is located off-site. However, plant steam may be used for humidification and general process use.
Again, the generation of steam should consider and mitigate any environmental impact.
7.4 Sustainable Construction
Construction involves activities including the use of building materials from various sources, use of various and multiple machines, demolition of existing structures, development on “green spaces”, removal of trees etc, all of which can impact environment in one or more ways.
Construction has a direct impact on the environment due to the following reasons:
- Generation of waste materials;
- Emissions from vehicles, machineries;
- Noise pollution due to use of heavy vehicles and construction machineries; and
- Releases of wastes and pollutants into water, ground and atmosphere.
A sustainability assessment of construction projects is essential to best ensure that it does not create any harmful effects on the living ecosystem while optimising the cost of construction.
In order to support sustainability during construction, the Contractor should be required to monitor and respond to some key criteria. This will include:
- Biodiversity Enhancement;
- Support to the Community;
- Effective Use of Resources;
- Pollution Reduction;
- Creating Healthy Environment; and
- Process Management.

